
3.2.2.
Matched analysis
Matching was successful for seven of the nine comparator
antimuscarinics; propiverine and darifenacin were not
considered because of small sample sizes. Persistence and
adherence outcomes for the matched comparisons are
presented in
Supplementary Tables 6–9 and 11–13
.
The median time to discontinuation (adjusted HR range
1.31–2.31;
p
<
0.0001 all comparisons) and 12-mo persis-
tence rates (adjusted OR range 0.18–0.71;
p
0.0001 all
comparisons) were statistically significantly greater with
mirabegron than with other antimuscarinics in all patients.
An increase in both persistence endpoints was also evident
for mirabegron compared to other antimuscarinics in the
three predefined patient subcohorts (
p
values 0.04 to
<
0.0001), except for 12-mo persistence versus solifenacin
in matched analysis of treatment-experienced patients. The
mean MPR was significantly greater with mirabegron than
with other antimuscarinics, except for solifenacin, in all
patients (
p
values 0.03 to
<
0.0001), and in treatment-naı¨ve
subcohorts, except for flavoxate (
p
values 0.02 to
<
0.0001).
4.
Discussion
In this study, patients prescribed mirabegron were signifi-
cantly more likely to continue treatment in the long term
compared to those prescribed tolterodine ER, with 12-mo
persistence rates of 38% and 20% and median times to
discontinuation of 169 and 56 d, respectively. Persistence
was also significantly greater with mirabegron than with
each of the other comparator antimuscarinics, including the
two most commonly prescribed antimuscarinic agents in
this large UK population, oxybutynin IR and solifenacin.
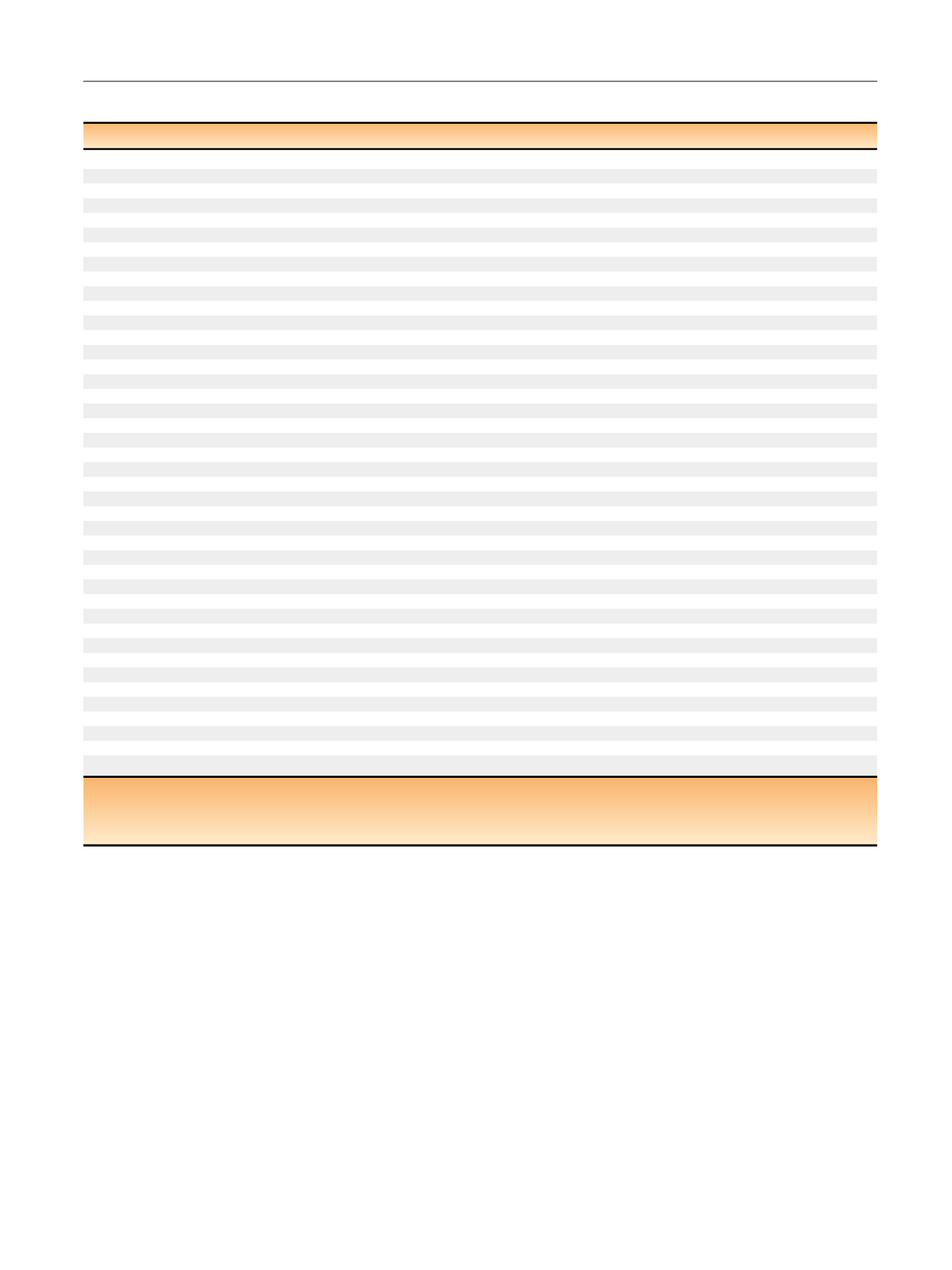
Table 3 – Persistence (time to discontinuation): multivariate Cox regression model (unmatched analysis)
Covariates
aHR (95% CI
) bp
value
Mirabegron versus tolterodine ER
Index drug
Mirabegron (reference)
–
–
Tolterodine ER
1.55 (1.41–1.71)
<
0.0001
Gender
Male (reference)
–
–
Female
0.96 (0.88–1.06)
0.44
Age in years
<
65 yr (reference)
–
–
65 yr
0.95 (0.87–1.04)
0.29
CCI score
0.95 (0.90–1.01)
0.09
Treatment status
Naı¨ve (reference)
–
–
Experienced
0.74 (0.68–0.82)
<
0.0001
Hypertension
No (reference)
–
–
Yes
0.90 (0.80–1.02)
0.10
Polypharmacy
a0 (reference)
–
–
1
0.98 (0.89–1.08)
0.67
2
0.78 (0.61–0.98)
0.04
3
0.66 (0.48–0.90)
0.01
4
0.88 (0.61–1.27)
0.49
Mirabegron versus antimuscarinics
Index drug
Mirabegron (reference)
–
–
Darifenacin
1.77 (1.45–2.16)
<
0.0001
Fesoterodine
1.38 (1.26–1.51)
<
0.0001
Flavoxate
2.27 (1.89–2.72)
<
0.0001
Oxybutynin ER
1.46 (1.33–1.60)
<
0.0001
Oxybutynin IR
1.90 (1.76–2.05)
<
0.0001
Propiverine
1.66 (1.31–2.10)
<
0.0001
Solifenacin
1.24 (1.15–1.34)
<
0.0001
Tolterodine IR
1.59 (1.46–1.74)
<
0.0001
Trospium chloride
1.58 (1.43–1.74)
<
0.0001
Gender
Male (reference)
–
–
Female
1.05 (0.90–1.16)
0.0075
Age
<
65 years (reference)
–
–
65 years
0.94 (0.86–1.09)
<
0.0001
CCI score
0.97 (0.89–1.03)
0.0006
Treatment status
Naı¨ve (reference)
–
–
Experienced
0.69 (0.67–0.72)
<
0.0001
Hypertension
No (reference)
–
–
Yes
0.92 (0.89–0.96)
0.15
Polypharmacy
b0 (reference)
–
–
1
1.03 (0.10–1.06)
0.0643
2
0.87 (0.80–0.94)
0.0003
3
0.81 (0.74–0.89)
<
0.0001
4
0.79 (0.69–0.89)
0.0004
CCI = Charlson comorbidity index; CI = confidence interval; ER = extended release; HR = hazard ratio; IR = immediate release.
a
HRs compared with reference variables for each covariate; HR
>
1 indicates an increased likelihood of discontinuation with the test variable versus the
reference variable.
b
Number of unique prescription drugs at the index date.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 3 8 9 – 3 9 9
395
















