
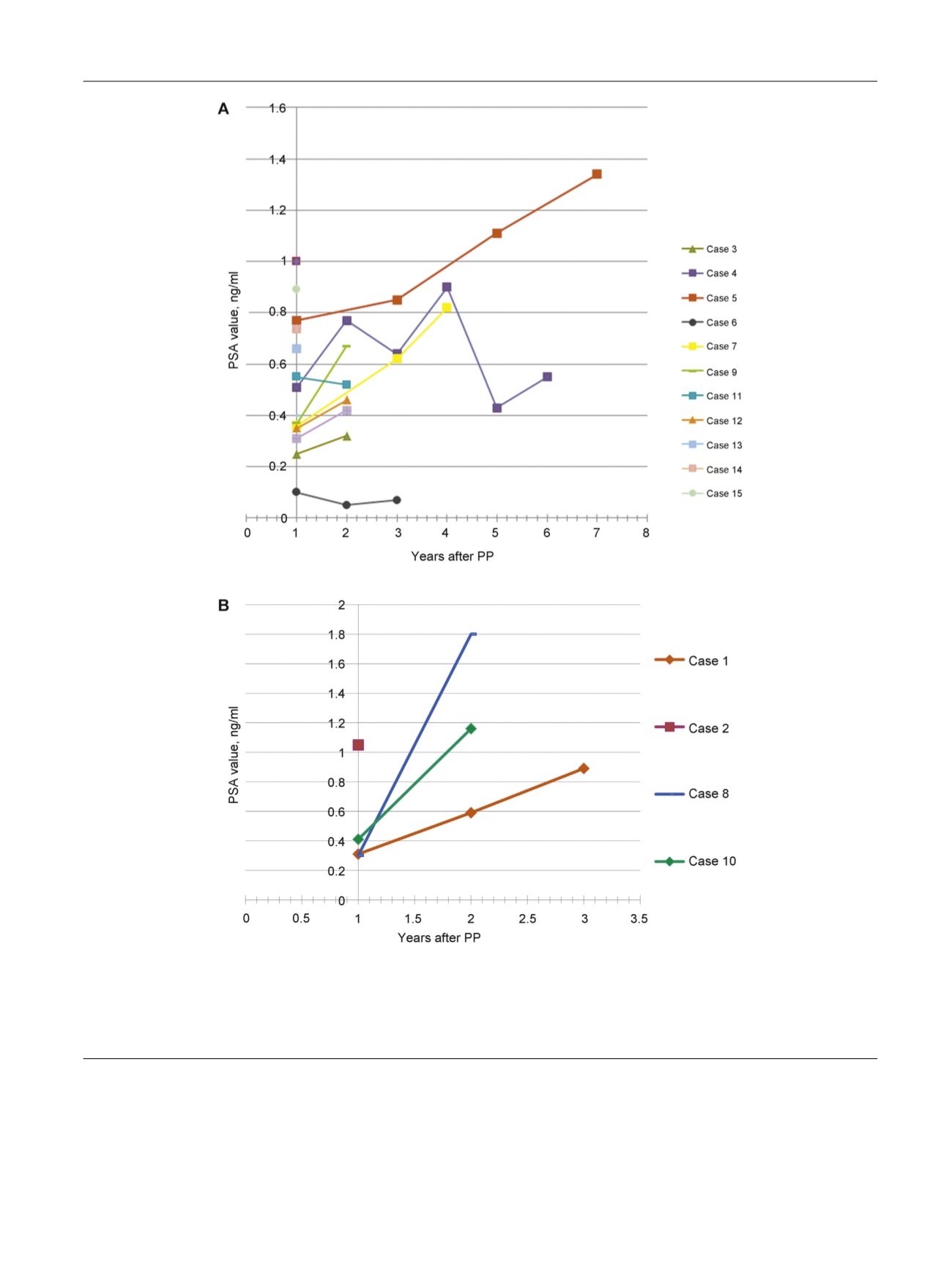
of this PSA rise over time
( Fig. 4 )with protocol-based biopsies
and MRI revealing no evidence of cancer. Of eight patients
with stage pT3a after APP, 3 (37%) had a cancer recurrence.
Among the nine pT2 cases, one (11%) was part of the four
patients who recurred. The APC recurrence rate was 17%, 30%,
and 0% for GS 6, 7 (3 + 4), and 7 (4 + 3) at RP, respectively.
A rising PSA suspicious for cancer occurred in 4 of 17men
(24%; cases 1, 2, 8, and 10)
( Fig. 3b) at 0.3, 2.5, 2, and 2 yr,
respectively
( Fig. 5). APC recurrence-free survival was 0.86
(range: 0.55–0.96) at 2 yr and 0.67 (range: 0.33–0.87) at
3 yr. MRI was suspicious and MRI-targeted biopsies were
positive, all at the area corresponding to the location of the
[(Fig._3)TD$FIG]
Fig. 3 – (a) Prostate-specific antigen (PSA) variations during follow-up starting from PSA nadir observed between months 3 and 9 postoperatively for
13 of 17 patients with no cancer recurrence. Cases 5, 7, and 9 showed slow PSA elevation and had residual benign prostatic hyperplasia at magnetic
resonance imaging and no cancer at biopsies. (b) PSA variations during follow-up starting from PSA nadir were observed between months 3 and
9 postoperatively for 4 of 17 patients who had cancer recurrence diagnosed at months 2, 24, 25, and 30. Three of four patients had complementary
radical prostatectomy with undetectable PSA postoperatively.
PP = partial prostatectomy; PSA = prostate-specific antigen.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 3 3 3 – 3 4 2
337
















