
complications. Pathology results are shown in
Table 3. In two
cases, an additional separate clinically insignificant PZ cancer
of 4 mm and 3 mm with GS 6 (3 + 3) was identified at
pathology at a location not in contact with the anterior
PZ margin site. No significant technical difficulties were
encountered during the posterolateral aspect of the prostate
dissection, posterior to the endopelvic fascia or in the
prerectal space. One patient (case 1) had Clavien-Dindo
grade 3b peritonitis due to spontaneous perforation of a
sigmoid diverticulum on day 7 (6%), requiring colectomy and
temporary colostomy. Two cases (7 and 15) had a focal
posterolateral margin, at risk for incomplete tumor resection.
3.4.
Functional outcomes
The pre- and postoperative questionnaire data are
shown in
Table 4 , Figure 6 ,and Supplementary
Figure 3. At 6–12 mo after surgery, potency remained
uninterrupted in 10 of 12 patients (83%) who were potent
preoperatively with an IIEF score 15, including one
patient who had salvage RP. Of the five remaining patients
with an IIEF score
<
15 preoperatively, two had improve-
ment with use of phosphodiesterase type 5 inhibitor drugs
with an IIEF score
>
15. Continence remained uninter-
rupted in all patients; however, three patients had
urgency for 2–3 mo.
4.
Discussion
We explored a surgical, in lieu of a thermal, focal treatment
option for highly selected consenting patients with anterior
apical PCa. Surgical treatment planning was based on
tumor location and intraprostatic anatomy derived from
mpMRI and targeted biopsy data. We leveraged our prior
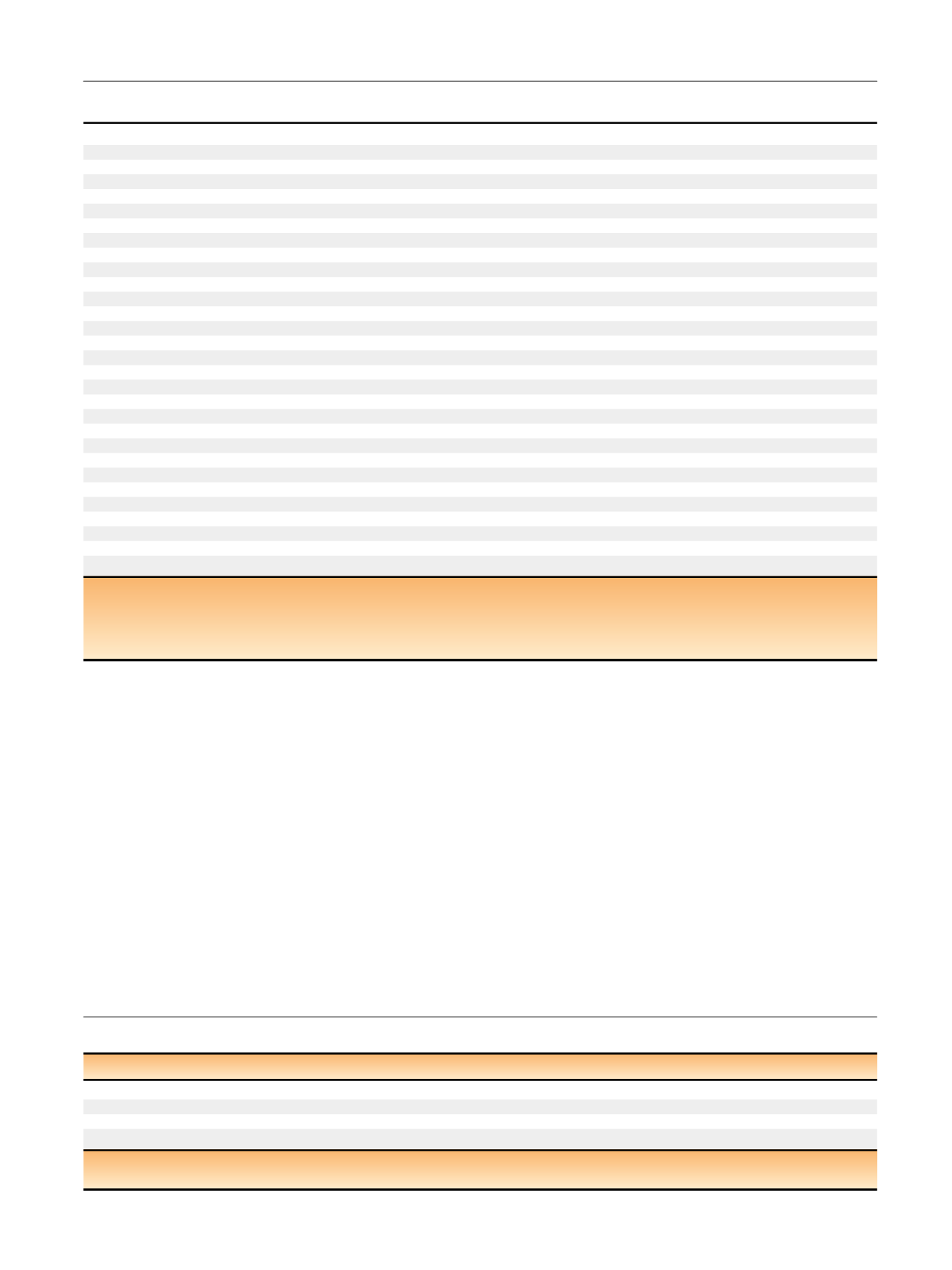
Table 4 – Functionnal outcomes based on urinary and sexual function questionnaires
Preoperative, median (IQR)
6–12 mo, median (IQR)
Difference between preoperative and 6–12 mo, median (95% CI)
ICS score
0 (0–0)
0 (0–4)
4 (1–7)
IPSS score
5 (0–11)
2 (0–4.5)
3 ( 2 to 10)
IIEF-5 score
19 (15–25)
20 (11–24)
4 ( 4 to 13)
No. of cases
16
14
CI = confidence interval; ICS = International Continence Society; IIEF = International Index of Erectile Function; IPSS = International Prostate Symptom Score;
IQR = interqartile range.
Table 3 – Biochemical and pathologic postoperative data and outcomes of the 17 patients included for anterior partial prostatectomy
Follow-up, mo, median (Q1–Q3)
30 (25–70)
Postoperative nadir PSA, ng/ml, median (Q1–Q3)
0.4 (0.3–0.7)
Pathology at partial prostatectomy specimen,
n
(%)
pT2
9 (53)
pT3a
8 (47
) *pN0 (average number of removed nodes: 6)
3 (100)
Margins
Anterior:
n
(%); length, mm, median (Q1–Q3)
5/17 (29); 4 (2–6)
Posterior/lateral:
n
(%); length, mm, median (Q1–Q3)
6/17 (35); 8 (2–35)
All margins,
n
(%)
9/17 (53
) **Cancer volume, cm
3
, median (Q1–Q3)
5.3 (3.5–7.1)
GS
6 (3 + 3)
6
7 (3 + 4)
10
7 (4 + 3)
1
MRI and biopsies
No. of cases with recurrence at postoperative protocol-based MRI at 1 yr
0/1
6 ***No. of cases with recurrence at protocol-based 12-core posterior systematic biopsies at 1 yr
1/
7 ****No. of cases with recurrence at postoperative for-cause targeted biopsy to lateral/postmargin area and/or MRI lesion
4/4
Positive targeted biopsy core cancer length, mm
Clinically insignificant cancer, GS 6 (3 + 3)
2
Clinically significant cancer, GS
7 (3 + 4)
6 and 5
7 (4 + 3)
2
Pathology at secondary RP, pT2a/N0 or pN0,
n
4/4
Positive margins at anterior aspect of specimen
2
Residual cancer largest dimension by GS, mm
6 (3 + 3)
2
7 (3 + 4)
8 and 20
7 (4 + 3)
7
GS = Gleason score; MRI = magnetic resonance imaging; PSA = prostate-specific antigen; Q = quartile; RP = radical prostatectomy.
*
Median follow-up was 40 mo (range: 28–61) for these nine cases with pT2 stage and 60 mo (range: 30–72) for these eight cases with pT3 stage.
**
Median follow-up of R0 PCa was 26 mo (range: 15–38). No patients recurred among these eight cases.
***
Most recent case 17 recurred in only 3 mo postoperatively.
****
Only the first six cases had postoperative protocol-based 12-core posterior systematic biopsies.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 3 3 3 – 3 4 2
339
















