
experience with mpMRI and targeted biopsies to precisely
identify APCs originating from the TZ.
Our group
[4]and others
[5,15,16]have published
precise morphometric and anatomic descriptions that led
us to explore this concept of APP in very carefully selected
patients after detailed informed consent.
In each of our cases, the TZ-originated cancer invaded, or
was entirely confined, to the AFMS. As such, simple
prostatectomy (BPH enucleation) would have been insuffi-
cient because it would not have excised the AFMS. We
learned that prostate volume (should be
>
42 cm
3
, which is
the 25th percentile of whole-gland volume of the no-
recurrence group) (Supplementary Fig. 2) is an important
factor for the success of the procedure. The technical
challenge of partial prostatectomy is not at the apex or at
the anterolateral aspect of the gland where the dissection
planes are similar to RP; the challenge is to ensure negative
margins posterolaterally at the PZ site. One patient (case 10)
with GS 7 (4 + 3) was included and was one of the four
patients who recurred. This inclusion criteria of the GS score
7 (4 + 3) or higher should be considered oncologically
incorrect. This case had a detectable PSA at 3 mo after RP
completion. Therefore selection criteria in the four men
who recurred were not so strict, and their results help refine
the selection criteria of patients as candidates for the
technique in future studies. Additional criteria for selection
should include whole-gland volume
>
40–45 cm
3
. The
technique may also include frozen section assessment of
the PZ margin.
Focal ablative therapy is a suboptimal treatment option
for PCa located in the anterior apex of the prostate because
of potential thermal diffusion injury to the external striated
sphincter, neurovascular bundles, and/or urethra, as well as
interference from the pubic symphysis. To the best of our
knowledge, the outcomes of focal high-intensity focal
ultrasound, cryotherapy, or laser ablation focusing on this
specific location are not available
[17] .We are acutely
aware that this concept of surgical focal excision is
controversial. This concept is open to the valid critiques
levied at focal ablation for PCa, such as uncertainty
regarding the natural history of untreated cancer foci,
uncertain post-treatment monitoring using PSA and MRI,
lack of long-term oncologic outcomes data in a larger
cohort, and lack of QOL data compared with traditional
treatment strategies
[18,19]. However, given that the
cancer lesion is surgically excised, it can be subjected to
accurate pathologic staging/grading, an aspect that is not
feasible with ablative partial/focal therapy
[20]. As for any
focal treatment, the remainder of the gland should be
devoid of any known foci of significant PCa, and it should be
possible to perform a completion of radical procedure in
case of recurrence or de novo cancer during follow-up.
However, a strength of our study is the meticulous reporting
of all relevant data regarding PSA, MRI, histopathology,
follow-up continence and potency questionnaires, and our
data with 30 mo of follow-up (range: 25–70).
This initial experience with robot-assisted APP provides
the following insights. First, the technique is feasible and
safe. Partial prostatectomy was not judged to be more
difficult than RP by the participating surgeons, all of whom
had expertise in robot-assisted surgery. Second, functional
outcomes were satisfactory. No patient reported stress
incontinence, in contrast to a 16% incontinence rate
following robot-assisted RP
[21]. Erectile function was
maintained at 6 mo in 10 of 12 men (83%) who were potent
preoperatively, which compares favorably with the 12-mo
potency rates of 54–90% after RP
[21]. Going forward, QOL
questionnaires should be added to assess overall benefits or
harms. Third, median PSA was 0.4 ng/ml (IQR: 0.3–0.7) at
3 mo. This value is close to the value of 0.6 ng/ml (range:
0–1.3) after a simple robot-assisted RP
[22], but lower,
probably because some of the PZ and most of the anterior
and apical prostate were resected. There is currently no
accepted definition for biochemical disease recurrence after
focal therapy
[23].
Fourth, our 29% anterior location rate of positive margins
(PMs) should be compared with RP anterior location rates,
in which the PZ was not preserved. However, our series is
made of highly selected cases that do not reflect the whole
spectrum of APC. Hence positive margin rates of 22%
anteriorly and 37% at the BN locations were observed in a
series of 55 RPs with TZ-originated cancer
[24]. A 46% rate of
PMs was observed in a series of 68 patients for which APC
[(Fig._6)TD$FIG]
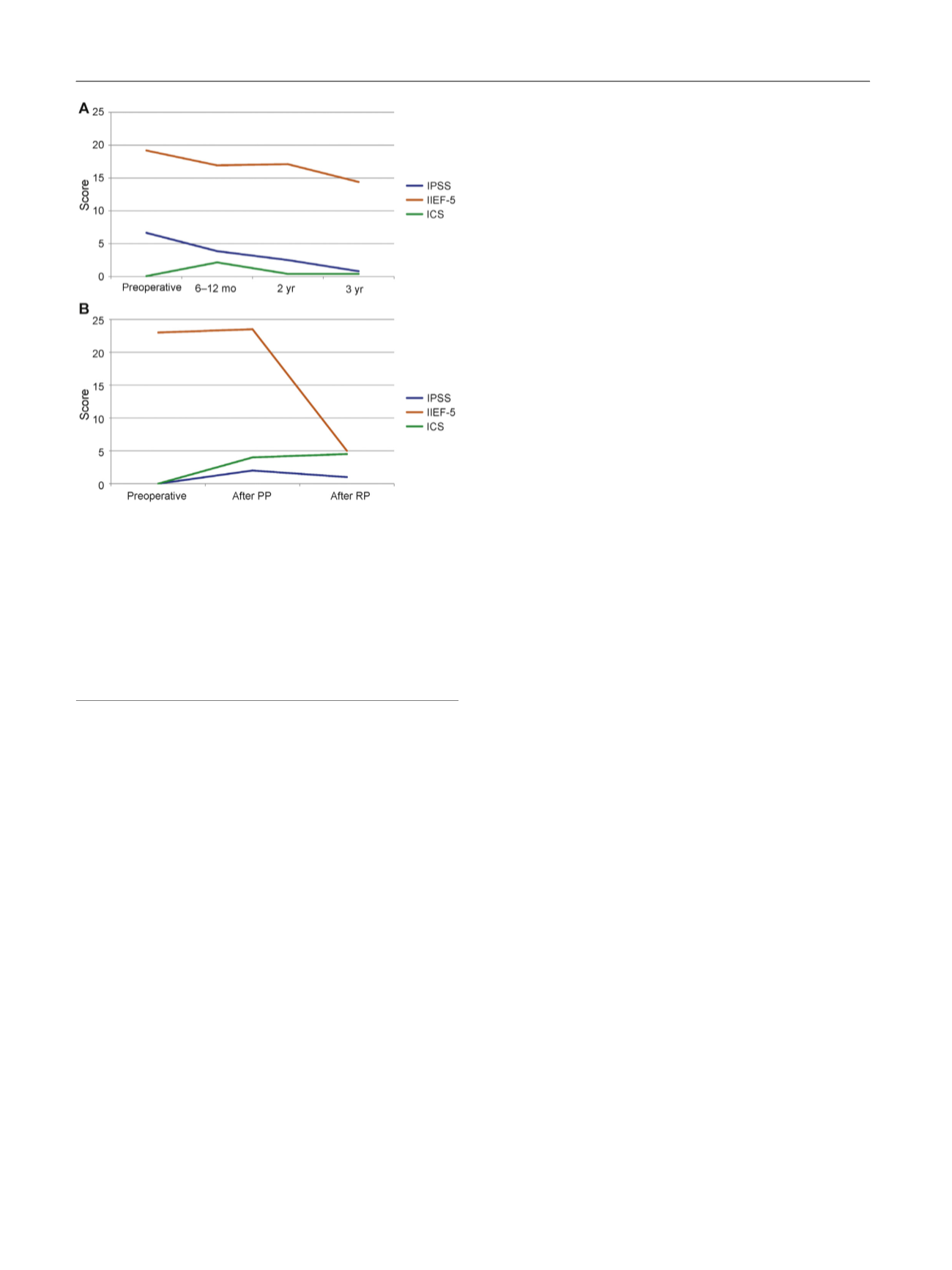
Fig. 6 – (a) Median International Prostate Symptom Score (IPSS),
International Index of Erectile Function (IIEF)-5, and International
Continence Society (ICS) scores from baseline to 3 yr. ICS score
remained almost unchanged with no incontinence. There is gradual
improvement of the median IPSS score and a gradual decrease of the
median IIEF-5 scores. (b) Median IPSS, IIEF-5, and ICS scores from
baseline to after anterior partial prostatectomy and to after complete
radical prostatectomy for the 4 of 17 patients who had cancer
recurrence diagnosed at months 2, 24, 25, and 30.
ICS = International Continence Society score; IIEF = International Index
of Erectile Function; IPSS = International Prostate Symptom Score;
PP = partial prostatectomy; RP = radical prostatectomy.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 3 3 3 – 3 4 2
340
















