
variables in the multivariable Cox regression analysis. The
progression score contained independent prognostic infor-
mation when compared to clinical risk factors and EORTC
risk scores
( Table 2 ). A nomogram for progression-free
survival (PFS) based on continuous EORTC risk and
progression scores is shown in
Fig. 3, together with an
associated calibration plot and receiver operating character-
istic (ROC) analysis for predicting 2-yr PFS. Combining the
progression and EORTC risk scores significantly increased
the predictive accuracy from 0.78 to 0.82 (
p
<
0.001). The
calibration plot shows substantial uncertainty for high
probabilities of progression, and the ROC analysis shows
that the combined score has better specificity at lower
sensitivities compared to the EORTC score, but is otherwise
very similar to clinical information alone.
In addition, we found that the progression score was
associated with previously identified classes in NMIBC
[15]. Tumours with high-risk progression scores were
classified mostly as class 2 (high risk), while tumours with
low-risk progression scores were classified mostly as class 1
(low risk) or class 3 (intermediate risk) (
p
= 3.2 10
22
[10_TD$DIFF]
,
x
2
test; Supplementary Table 2).
3.2.
12-gene progression score performance (all tumours
analysed)
The risk of progression may change during the disease
course, and recurrent and multifocal tumours may have
different biological properties. To mimic a potential clinical
use of the test, we classified patients using the highest score
obtained in the disease course for cases for which multiple
tumours were analysed (71 patients; 37 synchronous and
60 metachronous tumours in addition to the first tumour).
Using this approach, the progression score changed from
low risk to high risk (cut-off
optimal
) for 14 patients and
remained stable in 80% (57/71) of patients. The impact on
test performance using progression scores from all tumours
analysed is shown in Supplementary Table 3 and Supple-
mentary Table 4. An overview of assay performance using
the first tumour only and inclusion of later tumours is
shown in Supplementary Table 5. To address the impact of
analysing multiple tumours further, we performed a
multivariable time-dependent Cox regression analysis
including the maximum observed continuous EORTC risk
and progression score variables. We obtained a progression
score (continuous) hazard ratio (HR) of 1.81 (95% confi-
dence interval [CI] 1.32–2.48;
p
<
0.001) and an EORTC risk
(continuous) HR of 1.14 (95% CI 1.06–1.22;
p
[10_TD$DIFF]
<
0.001),
which are highly similar to the values presented in
Supplementary Table 4. Consequently, inclusion of all
tumours analysed did not have any large effect on the
overall test performance, partly because of the limited
number of patients included for whom multiple tumours
were analysed.
3.3.
Comparison of progression scores from paired FF and FFPE
tissues
To determine whether our findings using FF tumour tissue
might be translated to the standard clinical setting using
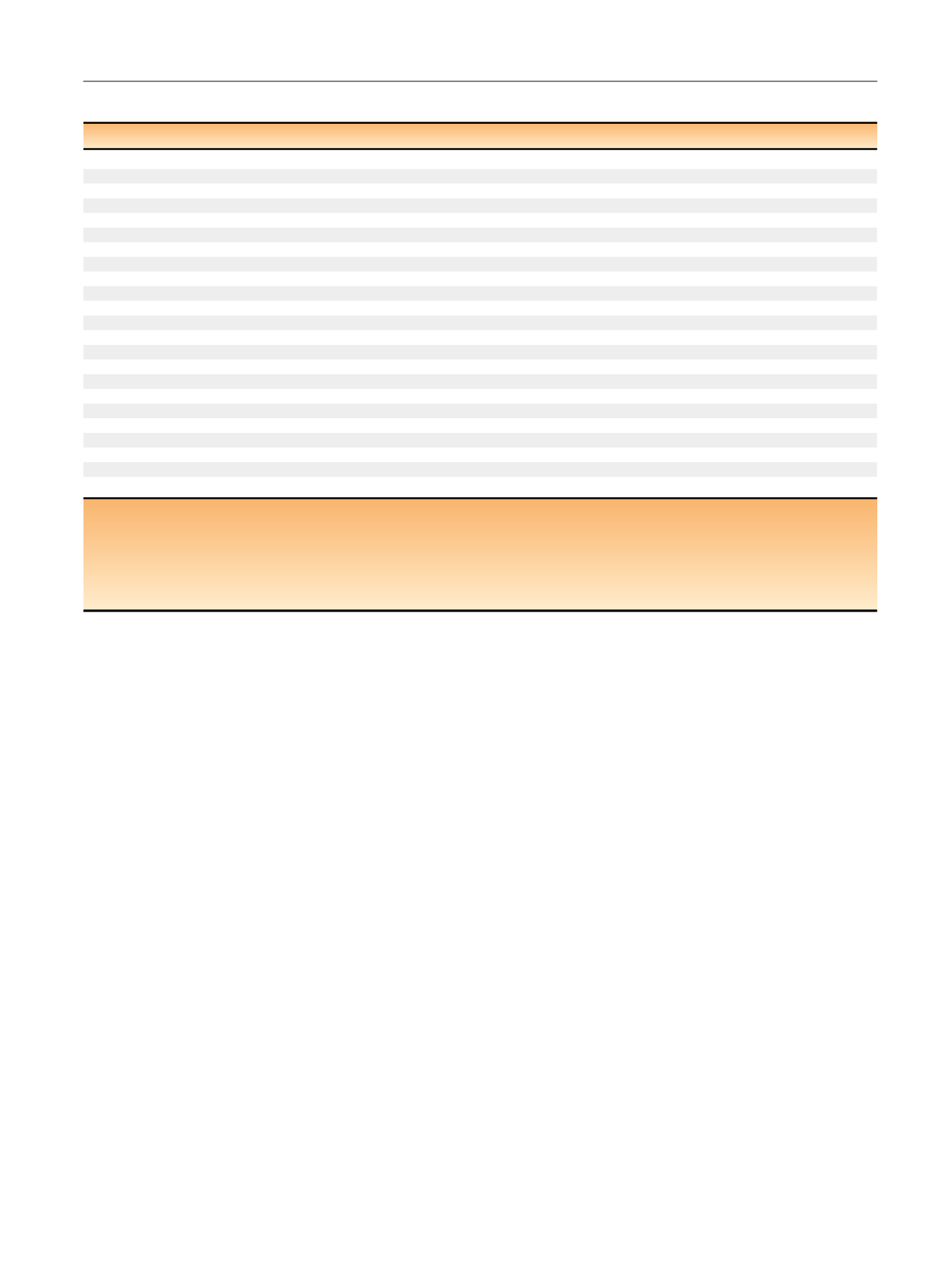
Table 2 – Cox regression analysis of progression-free survival with the first tumour in the disease course as the baseline
a[3_TD$DIFF]
HR (95% CI)
x
2
(df)
p
value
PA (%)
Univariate analysis (n = 578, 37 events)
Age
1.03 (1.00–1.06)
3.92 (1)
0.040
58.4
Gender (female vs male)
0.93 (0.43–2.05)
0.03 (1)
0.878
49.5
Stage (T1 + Cis vs Ta)
7.42 (3.67–15.04)
34.87 (1)
<0.001
75.5
Grade (high vs low + PUNLMP)
4.94 (2.32–10.51)
20.58 (1)
<0.001
70.1
Bacillus Calmette-Gue´rin (yes vs no)
0.63 (0.24–1.61)
1.07 (1)
0.329
53.8
Size ( 3 cm vs
<
3 cm)
1.40 (0.63–3.11)
0.63 (1)
0.415
53.2
Growth pattern (solid + mixed vs papillary)
4.45 (1.72–11.51)
6.70 (1)
0.002
55.5
Primary (yes vs no)
1.01 (0.53–1.93)
<
0.001 (1)
0.978
49.8
Multiplicity (multiple vs solitary)
1.48 (0.76–2.88)
1.29 (1)
0.248
53.0
Concomitant CIS (yes vs no)
3.59 (1.58–8.18)
7.03 (1)
0.002
56.5
EORTC risk score (
>
6 vs 6)
7.17 (3.28–15.71)
31.20 (1)
<0.001
73.3
EORTC risk score (continuous)
1.21 (1.14–1.28)
35.88 (1)
<0.001
78.4
Progression score (high vs low risk)
5.08 (2.23–11.57)
19.56 (1)
<0.001
68.1
[4_TD$DIFF]
Progression score (continuous)
2.39 (1.82–3.16)
41.85 (1)
<0.001
78.6
PA model (clinical)
81.8
PA model (clinical +
[4_TD$DIFF]
Progression score [continuous])
85.7
Multivariable model 1 (n = 517, 34 events)
55.84 (2)
<0.001
85.7
[4_TD$DIFF]
Progression score (continuous)
1.95 (1.44–2.65)
<0.001
Stage (T1 + CIS vs Ta)
4.21 (1.89–9.39)
<0.001
Multivariable model 2 (n = 578, 37 events)
53.36 (2)
<0.001
82.2
[4_TD$DIFF]
Progression score (continuous)
1.90 (1.39–2.58)
<0.001
EORTC risk (continuous)
1.13 (1.05–1.21)
0.001
HR = hazard ratio; CI = confidence interval; df = degrees of freedom; CIS = carcinoma in situ (concomitant); PA = prediction accuracy (Harrell’s concordance
index)
[1_TD$DIFF]
; PUNLMP = papillary urothelial neoplasm of low malignant potential; EORTC = European Organisation for Research and Treatment of Cancer.
a
[5_TD$DIFF]
For patients with
[6_TD$DIFF]
non progression
[2_TD$DIFF]
>
[7_TD$DIFF]
12 mo of follow-up were
[8_TD$DIFF]
required to be included in the analysis. The clinical PA model included age, stage, grade, growth
pattern, and CIS. Bold indicates
p
<
0.05. The HR for continuous
[4_TD$DIFF]
progression score and EORTC scores is for a 1-unit increase. Multivariable Cox regression model
1 shows model variables (
p
<
0.1) after backward selection from a model starting with all significant (
p
<
0.05) variables from univariate Cox regression analysis
(ie, age, stage, grade, growth pattern, and concomitant CIS). Multivariable Cox regression model 2 included the
[4_TD$DIFF]
progression score and EORTC risk score only. All
variables were measured at the time of transurethral resection of the bladder.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 4 6 1 – 4 6 9
465
















