
initiatives. Moreover, without validated QIs it is difficult to
ascertain the true degree of quality variations and
importantly, the impact this variation has on patient
outcomes. Herein, we developed case-mix adjusted QIs to
benchmark RCC surgical quality of care at a hospital-level.
Utilizing these tools we reveal the wide variations in care
that patients experience, and further demonstrate the
negative consequence of this variation on important patient
outcomes.
To the best of our knowledge, these results are the first to
display widespread variability in the care that patients
receive on a national level when undergoing RCC surgery
while adequately adjusting for case-mix variation. While
Gore et al
[17]have previously demonstrated hospital-level
variation in quality following radical nephrectomy in the
state of Washington, this analysis suffered from case-mix
bias as tumor specific factors were not adjusted for. Notably,
our analysis revealed significant variations across all QIs,
[(Fig._4)TD$FIG]
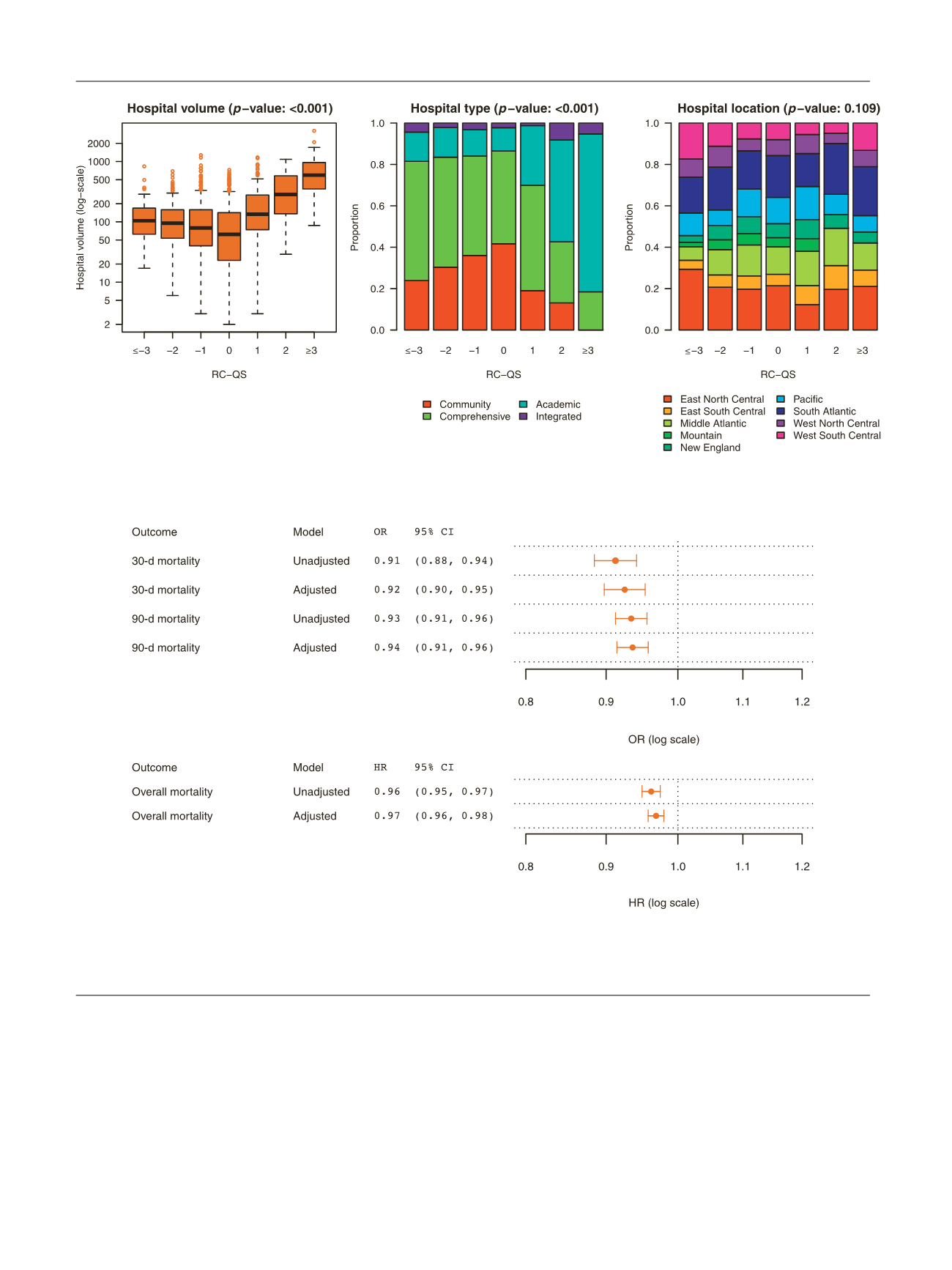
Fig. 4 – Impact of hospital quality on patient mortality. Unadjusted and case-mix adjusted associations between hospital quality, measured by the Renal
Cancer Quality Score (sum score), and 30-d, 90-d, and overall mortality. Note, values displayed reflect OR (odds ratio) and HR (hazard ratio) per 1 unit
change in Renal Cancer Quality Score.
CI = confidence interval.
Fig. 3 – Structural features associated with hospital quality. Associations between hospital quality, measured by the Renal Cancer Quality Score (RC-QS;
sum score), and hospital volume (left), type (middle) and geographical location (right).
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 3 7 9 – 3 8 6
384
















