
where S stands for the standard error of the observed outcome
[35_TD$DIFF]
O, taking
the model-based expected outcome E to be a fixed quantity, and
calculated
p
-values from the standard normal distribution.
For each QI, we classified outlier hospitals performing worse than
expected as poor outliers and those performing better than expected as
superior outliers. We experimented with adjusting for multiple testing
through Bonferroni correction and control of false discovery rate
[15],
but chose to use the fixed
p
-value threshold of 0.05 for the purpose of
classifying outlier hospitals for further analyses as previously reported
[10,12]. Additionally, for data representation, we multiplied the
observed to expected outcomes ratio for each hospital by the national
average to determine the case-mix adjusted QI
[13_TD$DIFF]
[14]. Internal consistency
of the resulting outlier classifications was investigated via Venn
diagrams, pairwise Kendall’s tau correlations, and Cronbach
a
statistic.
Patients treated in outlier versus nonoutlier hospitals were compared by
30-d mortality, 90-d mortality (logistic regression), and overall mortality
(Cox regression). Mortality models were fitted using generalized
estimating equations allowing for within-hospital correlation, both
with and without case-mix adjustment. We calculated a composite
quality measure encompassing hospital performance across the five QIs,
hereafter referred to as the Renal Cancer Quality Score (RC-QS). Briefly,
for each QI a hospital
[14_TD$DIFF]
identified as a superior outlier
[15_TD$DIFF]
received one point,
for being a poor outlier one point was deducted, and for being a
nonoutlier zero points were awarded. The final RC-QS was a summation
of the points received across each indicator for an individual hospital. We
investigated the association of the RC-QS to outcomes using similar
regression models as described above, as well as to hospital location,
volume, and type of institution. Statistical
p
-values for the hospital
characteristics associations were calculated from chi-square (location)
and two-sample Wilcoxon tests (volume and type), comparing hospitals
with positive sum scores to hospitals with negative sum scores, omitting
zero scores. The statistical analyses were performed in SAS software
version 9.3 (SAS Institute, NC, USA) and R statistical environment version
3.2.2 (R Foundation for Statistical Computing, Vienna, Austria).
3.
Results
Variations in the quality of RCC surgical care were captured
across five QIs: MIS, PN, PM, LOS, and RP. The number of
patients analyzed for each QI and their corresponding
comorbidities, tumor-, and treatment-related characteris-
tics are summarized in
Table 1 .Statistically significant
interhospital variation was observed for all QIs (
p
<
0.001)
with random effects models indicating between hospital
variance proportions of 31%, 17%, 12%, 15%, and 20% for the
MIS, PN, PM, LOS, and RP indicators, respectively. All of the
random effects remained significant when adjusting for
case-mix (
p
<
0.001). For each QI, more than 1100 hospitals
were benchmarked for quality performance against the
national average utilizing our case-mix adjusted QIs. A total
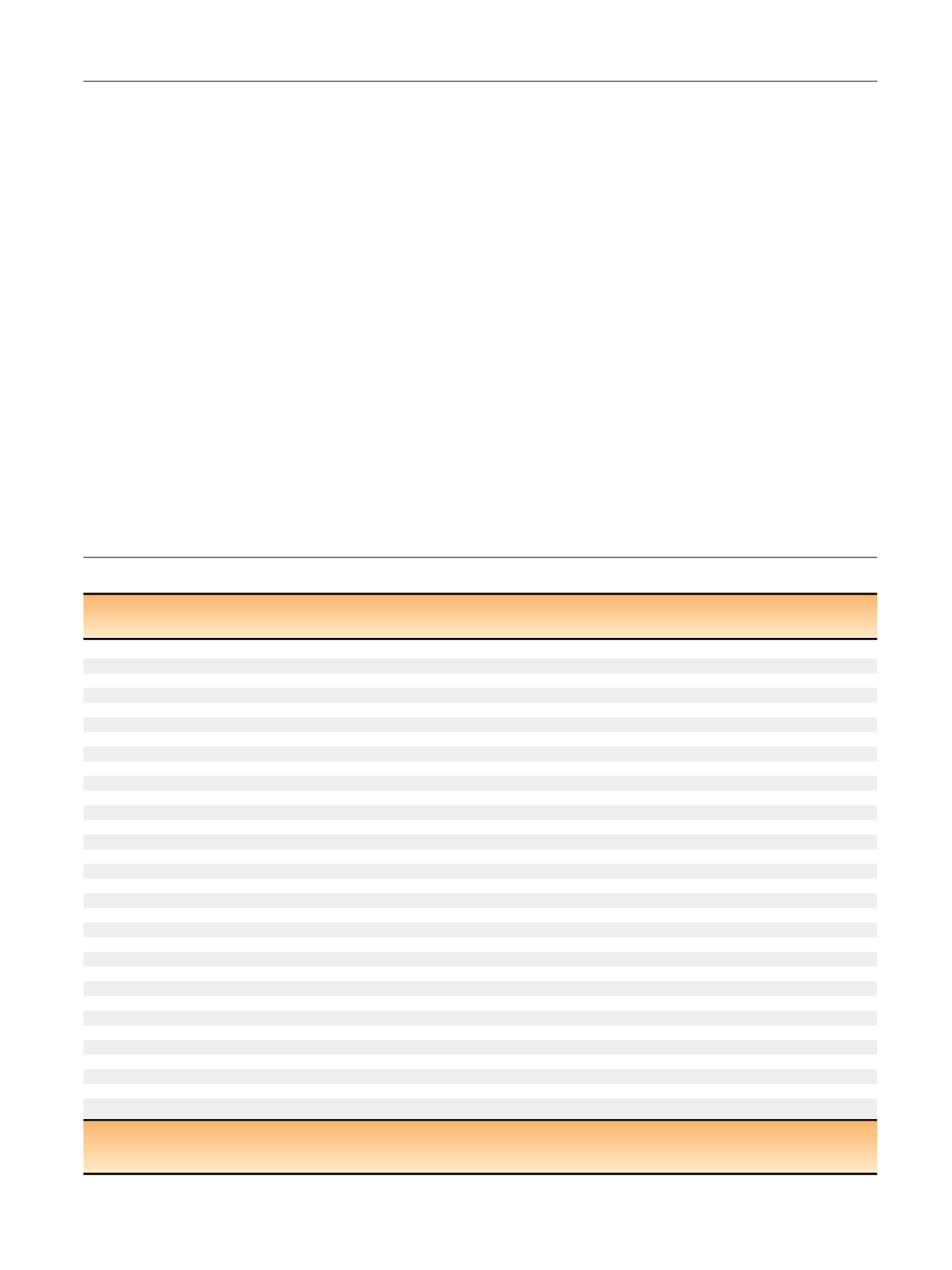
Table 1 – Study cohort characteristics
MIS
PN
PM
LOS
[31_TD$DIFF]
RP
Total (%)
Total (%)
Total (%)
Total (%)
Total (%)
N
a
34 150
87 408
71 422
126 289
131 319
Median age, yr (IQR)
62 (53–70)
60 (51–69)
59 (50–68)
62 (53–71)
62 (53–71)
Sex
Male
20 740 (61)
51 833 (59)
43 639 (61)
78 579 (62)
81 804 (62)
Charlson/Deyo Score
0
23 357 (68)
61 512 (70)
51 153 (72)
87 665 (69)
91 613 (70)
[32_TD$DIFF]
1
7834 (23)
19 487 (22)
15 748 (22)
28 657 (23)
29 520 (22)
[33_TD$DIFF]
2
2959 (9)
6409 (8)
4521 (6)
9967 (8)
10 186 (8)
T-Stage
T1
26 050 (76)
87 408 (T1a: 100)
71 422 (100)
69 134 (55)
71 517 (54)
T2
8100 (24)
NA
NA
20 994 (17)
21 803 (17)
T3
NA
NA
NA
34 253 (27)
35 962 (27)
T4
NA
NA
NA
1908 (1)
2037 (2)
Lymph node status
NX
29951 (88)
83341 (95)
68976 (96)
102245 (81)
106061 (81)
N0
3878 (11)
3935 (4)
2389 (3)
19149 (15)
20036 (15)
N1
321 (1)
132 (1)
57 (1)
4895 (4)
5222 (4)
Metastases
M0
NA
NA
NA
117 121 (93)
122 240 (92)
M1
9168 (7)
9990 (8)
Histology
Clear cell
[5_TD$DIFF]
27 010 (79)
68 277 (78)
54 022 (76)
103 320 (82)
107 555 (82)
Papillary
[6_TD$DIFF]
4548 (13)
13 419 (15)
12 326 (17)
13 104 (10)
13 549 (10)
Chromophobe
[7_TD$DIFF]
2195 (6)
4618 (5)
4214 (6)
6467 (5)
6643 (5)
Other
[8_TD$DIFF]
397 (2)
1094 (1)
860 (1)
3398 (3)
3572 (3)
Median tumor size, cm (IQR)
5.0 (3.5–7.0)
2.6 (2.0–3.4)
2.6 (2.0–3.6)
5.5 (3.7–8.0)
5.5 (3.8–8.1)
Tumor grade
G1/2
18 562 (54)
59 073 (67)
47 090 (66)
65 746 (52)
67 846 (52)
G3/4
8807 (26)
14 604 (17)
12 367 (17)
43 125 (34)
44 855 (34)
GX
6855 (20)
13 731 (16)
11 965 (17)
17 418 (14)
18 618 (14)
Median yr of diagnosis (IQR)
2011 (2010–2012)
2009 (2007–2012)
2010 (2007–2012)
2008 (2006–2011)
2008 (2006–2011)
No. hospitals assessed
1155
1207
1131
1245
1254
a
[4_TD$DIFF]
Denotes number of patients included in the analysis for each quality indicator.
IQR = interquartile range; LOS = length of stay; MIS = T1-2 tumors receiving a minimally invasive (laparoscopic or robotic) approach for radical nephrectomy;
NA = not applicable; PM = positive surgical margin following PN for T1 tumors; PN = T1a tumors undergoing partial nephrectomy.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 3 7 9 – 3 8 6
381
















