
sought to evaluate whether the change in clinical risk,
assessed from initial biopsy to final surveillance biopsy,
predicted the presence of adverse pathologic findings at
delayed radical prostatectomy (RP).
We identified study participants under a prior University
of California, San Francisco (UCSF) institutional review
board–approved protocol. Most men were selected based
on strict UCSF AS criteria: PSA 10 ng/mL, clinical stage T2
or lower, 33% positive biopsy cores, and 50% positivity
within a single core. Patients with relatively favorable risk
profiles outside of strict AS criteria (eg, higher volume
Gleason 3 + 3, low-volume Gleason 3 + 4) desiring surveil-
lance were also included. All pathology slides obtained from
outside institutions were reviewed by experienced aca-
demic pathologists. Men on AS between 1993 and 2013 who
consented to prospective data collection and who did not
receive definitive treatment for a minimum of 6 mo were
included and participated in a surveillance program, as
previously reported
[2]. The Cancer of the Prostate Risk
Assessment (CAPRA) score, an extensively validated risk
assessment instrument, was calculated, as described
previously, for all patients at initial diagnosis and following
most recent biopsy (Supplementary Table 1)
[3,4]. Patients
with high-risk PCa (CAPRA
>
5 and/or Gleason score 4 + 3)
at diagnosis and those without subsequent clinical follow-
up at our institution were excluded.
We evaluated the change in CAPRA score and its
constituent components among all patients from diagnosis
to last follow-up biopsy, using descriptive statistics and
contingency tables with
p
values based on chi-square tests.
Definitive treatment included RP, radiation therapy, andro-
gen deprivation therapy alone, or ablative therapy. Among
patients who received RP, adverse pathology was defined as
the presence of primary Gleason pattern 4 + 3, pathologi-
cal T stage T3a or higher, and/or lymph node positivity—
pathologic end points demonstrated to predict significant
future clinical events
[5] .The difference in CAPRA score
from diagnosis to last biopsy was then used as a primary
explanatory variable. A patient with, for example, a CAPRA
score of 1 on diagnostic biopsy and 4 on a third surveillance
biopsy would experience a net change of 3 points. Other
covariates that could affect the response variable were
included in the models, including PSA density, CAPRA score
at the time of last biopsy, and time from diagnosis to
prostatectomy. Among patients ultimately receiving
delayed RP, we used receiver operating characteristic
analysis to compare the effect of individual clinical
parameter reclassification with CAPRA score change on
the prediction of adverse pathology. Mann-Whitney
U
statistics were used to compare the area under the curve
(AUC).
Overall, 735 patients met the inclusion criteria and were
followed for a median of 52 mo. Mean age at diagnosis was
62 yr, and the median PSA was 5.2 ng/ml. At diagnosis,
577 patients (79%) met strict UCSF AS criteria, and 85% were
low risk (CAPRA 0–2), whereas 15% were classified as
intermediate risk (CAPRA 3–5). The complete baseline
clinical and demographic characteristics of the cohort
are shown in Supplementary Table 2. When assessed on
a continuous scale, CAPRA score was unchanged in
192 patients and decreased in 74. Shift in CAPRA score
occurred due to multidirectional changes in biopsy Gleason
score in 413 patients (56%), in PSA in 297 (40%), and in
percentage of positive cores in 278 (38%). Moreover, 97
(13%) experienced reclassification by Gleason score alone,
156 (21%)
[1_TD$DIFF]
by PSA alone, and 29 (4%) were reclassified based
on
[5_TD$DIFF]
changes
[6_TD$DIFF]
in tumor volume. In total, 282 (38%) had a
change in one parameter alone, 166 (23%) had changes in
two parameters, and 42 (5.7%) had changes in three
parameters
( Fig. 1). In a multivariable logistic regression
model, unit increases in CAPRA score were significantly
associated with the occurrence of adverse pathology (odds
ratio [OR]: 1.60; 95% confidence interval [CI], 1.25–2.04;
p
<
0.001). In addition, clinical risk (CAPRA) following last
biopsy was also independently associated with adverse
pathology (OR: 1.52; 95% CI, 1.21–1.92;
p
<
0.001)
( Table 1).
Magnitude of CAPRA score change (AUC: 0.72) outper-
formed individual PSA progression (AUC: 0.64;
p
= 0.03),
and change in percentage of cores positive for cancer (AUC:
0.64;
p
= 0.04) for the prediction of adverse pathology at
delayed RP.
Numerous surrogate end points during surveillance have
been proposed to identify individuals at risk for harboring
sufficiently aggressive disease warranting treatment.
Changes in biopsy Gleason grade or tumor volume are
widely regarded by surveillance protocols as an indication to
pursue treatment; these events occur in a reliable proportion
of men with each successive biopsy
[6,7] .The occurrence of
Gleason grade reclassification has been attributed to several
factors including the detection of higher grade or volume
tumor as a consequence of initial biopsy inaccuracy and the
contribution of genuine cancer progression over time;
however, the directionality of sampling limitations does
not uniformly favor underdetection
.
This has been reflected
in RP series in which misclassification at initial biopsy has
resulted in both pathologic upgrade and downgrade
[8] .Con-
sequently, reclassification metrics based solely on a single
clinical parameter may incompletely account for an individ-
ual’s risk of clinically significant disease progression and
expose many to early treatment.
We evaluated the change in clinical risk among men with
low- and intermediate-risk PCa managed with AS at a single
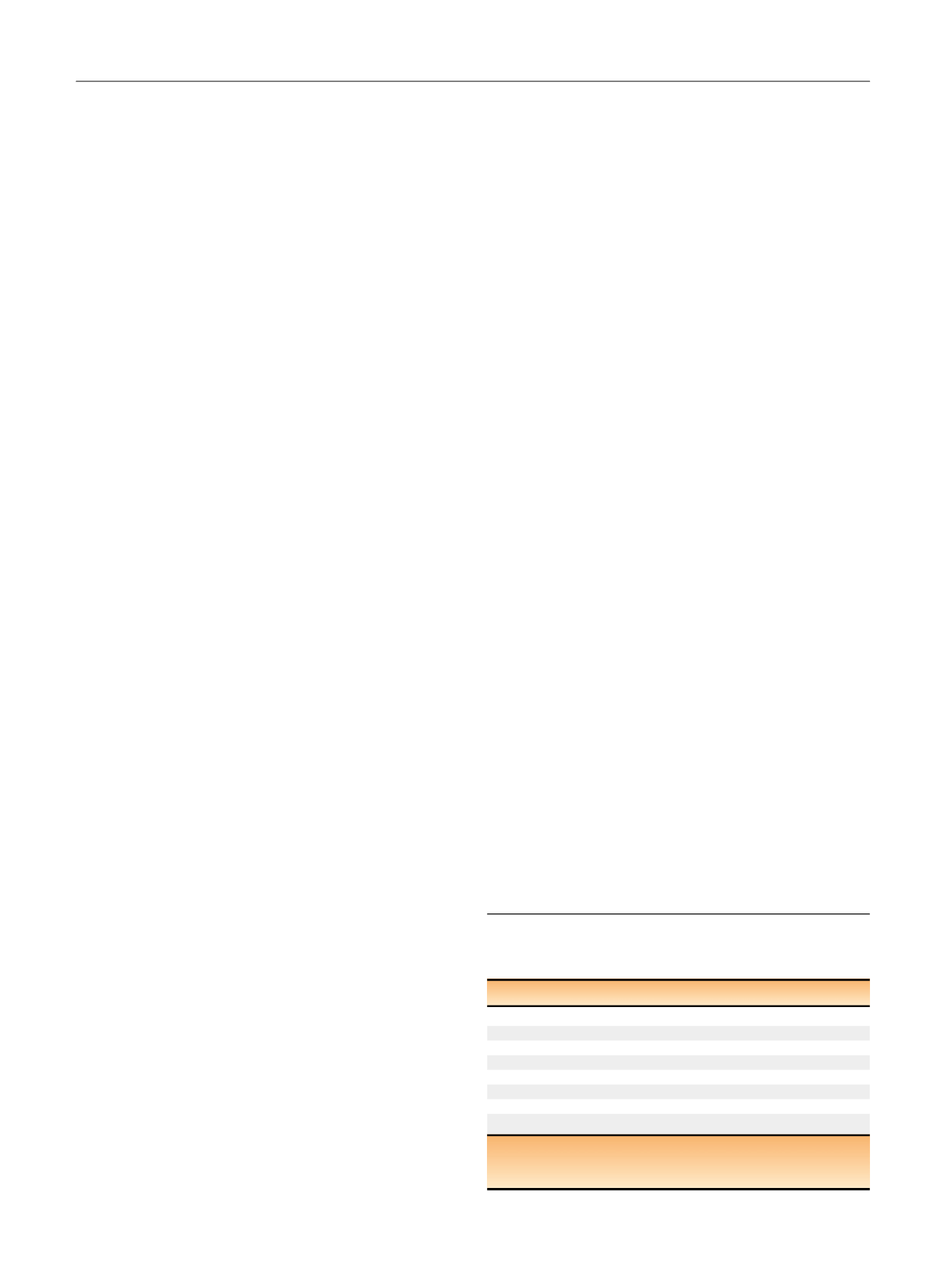
Table 1 – Multivariable logistic regression models of adverse
surgical pathology among men treated with radical prostatectomy
following initial active surveillance (
n
= 169)
Variable
OR 95% CI
p
value
CAPRA score at last biopsy (per 1 U)
1.52 1.21–1.92
<
0.001
Log PSA density
0.83 0.44–1.58
0.57
Age (per 5 yr)
1.15 0.89–1.49
0.29
Time to RP (yr)
1.17 0.99–1.39
0.07
Magnitude of CAPRA change (per 1 U)
1.60 1.25–2.04
<
0.001
Log PSA density
0.96 0.52–1.80
0.91
Age (per 5 yr)
1.24 0.96–1.61
0.10
Time to RP (yr)
1.18 0.99–1.39
0.06
CAPRA = Cancer of the Prostate Risk Assessment; CI = confidence interval;
OR = odds ratio;
PSA = prostate-specific antigen;
RP = radical
prostatectomy.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 3 2 9 – 3 3 2
330
















