
The findings in this study provide an important
pathophysiologic context to previous reports that active
surveillance for GS6 prostate cancer is highly effective and
safe. For example, in a cohort of 1300 men at the Johns
Hopkins Hospital, men with low-risk prostate cancer had
excellent outcomes on active surveillance, with 15-yr
metastasis-free and cancer-specific survival rates of 99.4%
and 99.9%, respectively
[21]. Other observational cohort
series with variable inclusion criteria and follow-up
duration have generally shown similar long-term outcomes
[22,23]. These findings are logically supported by the rarity
of adverse pathology for true GS6 in our study. The
favorable outcomes on active surveillance have led to
increasing rates of this management strategy for men with
low-risk prostate cancer, with recent studies showing
favorable outcome rates of 50%
[6,7]. Following maximal
characterization of the prostate cancer, routine treatments
of low-risk cancers with surgery or radiation are unlikely to
have a meaningful impact on long-term cancer-specific
survival, while exposing the patient to potential side effects
including sexual, urinary, and bowel dysfunction
[8]. Fur-
ther prospective studies of techniques to more accurately
image and diagnose prostate cancer on biopsy will provide
valuable information for patients and clinicians in finalizing
a management decision.
Limitations of our study include its retrospective design
and other potential biases. The RP cases fromeach institution
were reviewed separately, without assessing interobserver
agreement. Although the majority (60%) of GS6 cases did not
include a pelvic lymph-node dissection, and some lymph-
node metastases could theoretically have been missed, data
fromRoss et al in over 14 000 RPs suggest that this is unlikely
[1] .Our cohort included partial embedding of RP specimens,
and this may have led to incomplete data. Reasons for partial
embedding at both institutions were cost and burden to
pathology staff, similar to those reported by Vainer et al who
observed a decrease in workload of 30% for partial compared
to complete embedding, and who noted that only two of
238 prostatectomies (0.8%) were upstaged to pT3a because of
focal EPE that was only identified in the withheld part of the
specimens not originally examined
[24] .In another study,
Kim et al compared partial and complete embedding in
136 prostatectomy specimens, and there was perfect
agreement in detection rates for EPE using their reported
technique for partial embedding
[25]. The non-embedded
portions of the prostatectomy specimens in this study were
not available for retrieval and analysis because they had been
previously discarded as per institutional policy (retention for
6 months after the initial pathologic analysis). Fifteen (20%)
patients with GS6 pT3 and 21 (14%) with GS 7 pT3b had no
available pathology specimens, similar to the 14% rate of
unavailable specimens in the study by Ross et al
[1] .These
missing specimens and the non-embedded portions of
prostate tissue could have contained GS6 with EPE or SVI,
thus introducing a possible selection bias that could limit
external validity. The pathologists in this study were blinded
to patient information and previous pathology reports,
although they were aware of the purpose of the study as
well as the grade and stage of the cases being re-reviewed,
and this could have introduced bias. However, the large
sample size and multi-institutional nature of this study are
strengths. Further studies from other cohorts will evaluate
the incidence of ECE or SVI for GS6 prostate cancer, and this
will carry implications regarding the malignant potential of
true GS6. Hernandez et al previously reported no distant
metastases or mortalities attributed to prostate cancer in
over 2500 patients with GS6 pT2 disease, with a 1.3%
actuarial probability for 15-yr biochemical recurrence
[26] .With median follow-up of 20 mo, there were no cases
of biochemical recurrence for the seven patients with pT3a
and true GS6 in this study. In particular, genomics, molecular
profiles, and longer-term outcomes of biochemical recur-
rence, distant metastases, and prostate cancer-specific
mortality in patients with GS6 pT3a disease will be of
interest for future studies.
Both institutions in this study have had dedicated
genitourinary pathologists: University of Chicago since
2006, and Northwestern University since 2000. The changes
in grading and staging of specimens in this study on re-
review emphasize the challenge of pathologic assignment,
even at large academic centers with expert pathologists.
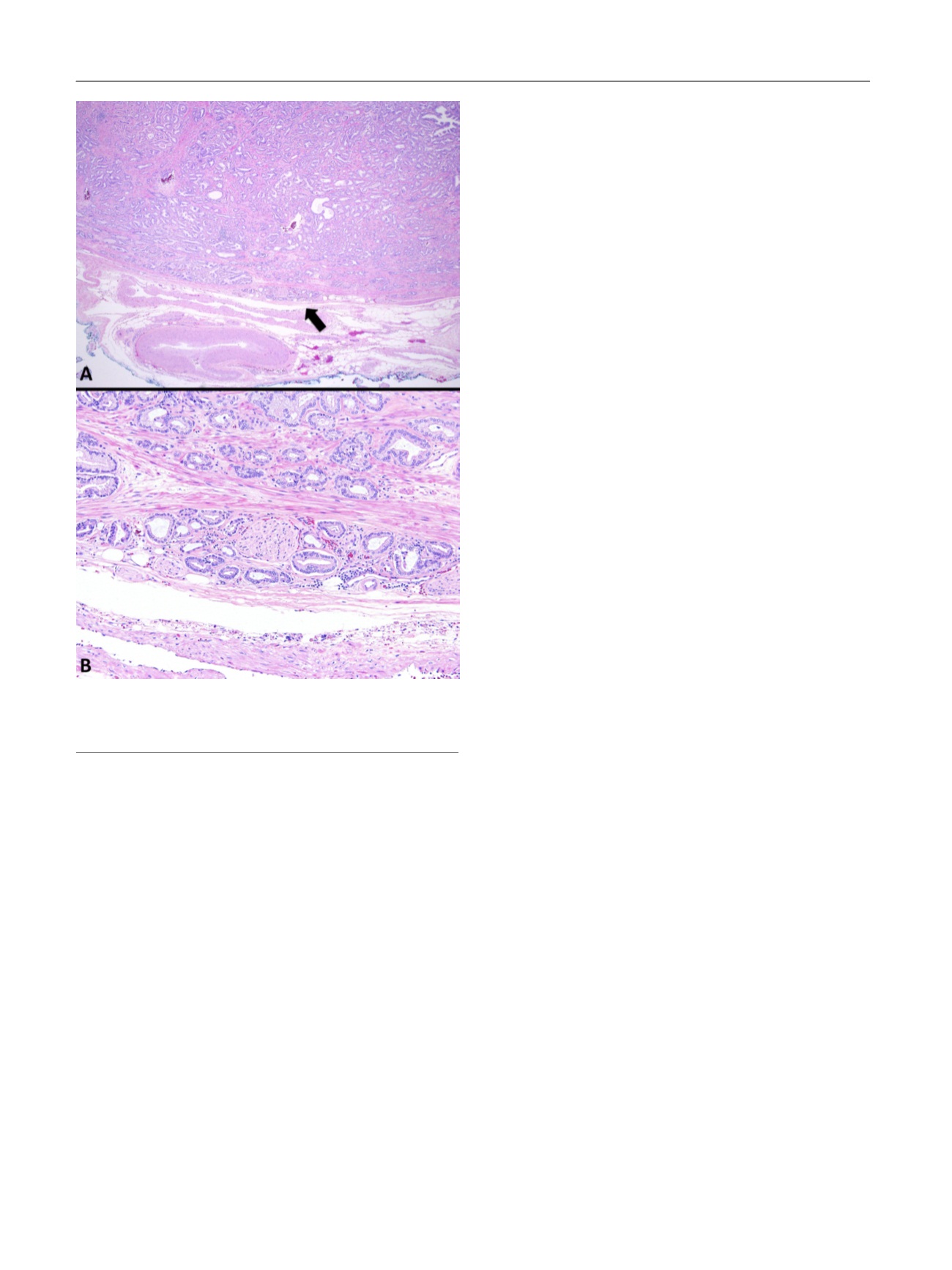
[(Fig._1)TD$FIG]
Fig. 1 – (A) Gleason score 6 (GS6) disease with focal extraprostatic
extension (EPE; arrow and B). (B) Neoplastic well-formed glands are
seen at the level of the adipocytes.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 4 5 5 – 4 6 0
458
















