
6 cancer. We found that when the kallikreins were assessed
before the initial surveillance biopsy (sometimes called the
confirmatory biopsy), the 4Kpanel provided incremental
benefit for prediction of high-grade cancer (Gleason 7)
over the clinical factors that are available at diagnosis.
Specifically, depending on the choice from the various
cutpoints that are based on the risk of high-grade disease, a
substantial number of biopsies could be avoided while
minimizing the number of missed high-grade cancers, few
of which had primary pattern 4. The 4Kpanel was not of
value over PSA for the prediction of reclassification in
subsequent biopsies after the first surveillance biopsy. We
found that the impact of other biopsy information,
primarily volume of core involvement in previous biopsies
and the number of previous negative biopsies, carries such a
statistical weight in modeling that the impact of the
4Kpanel is minimized. For example, if a patient had low-
volume disease at the initial surveillance biopsy or had
subsequent negative biopsies after the initial diagnosis,
then these factors were highly protective against biopsy
reclassification at subsequent biopsy. It should be noted
that our analysis of these subsequent biopsies used the
4Kpanel from the plasma sample that was closest to the
subsequent biopsy, not necessarily the plasma sample from
study entry, which could be months or years earlier than the
subsequent biopsy.
We included serum PSA and prostate volume separately
in our models instead of calculating PSA density, as we find
a better model fit when the variables enter the model
independently. While transurethral ultrasound prostate
volume measurements may suffer from imprecision
[16],
statistical models that included prostate volume appeared
to provide slightly improved predictive performance (AUC
for all groups 0.77 with volume vs 0.75 without volume).
Furthermore, prostate volume is a strong predictor of
finding higher-grade cancers, with larger prostates being
protective, as previously reported
[17].
This study has limitations that merit mention. First, the
model was developed and tested in the same cohort and
with relatively limited numbers that resulted in wide
confidence intervals and minor differences between the
training and test sets. The results should clearly be validated
in other cohort before clinical application. However, we
expect that our results will be similar to those found in a
community setting, as PASS is a multicenter center study
that represents a broad spectrum of men utilizing active
surveillance. Similarly, as PASS is primarily a Caucasian
cohort, the findings of this study may not be generalizable
to African American patients. Another limitation is that the
serum PSA measurements used were obtained as part of
standard clinical care, and the local site assays may differ
from the one used with the 4Kpanel. Thus, the comparative
modeling using PSA versus 4Kpanel may have slightly
different tPSA values, with caution suggested for compar-
isons between the models. Lastly, as the use of imaging such
as multiparametric MRI (mpMRI) is increasing, we do not
have MRI data for most of our participants and recognize the
potential value of future studies incorporating results from
mpMRI and biomarkers in active surveillance.
5.
Conclusions
The 4Kpanel was significantly associated with reclassifica-
tion at the first surveillance biopsy, providing incremental
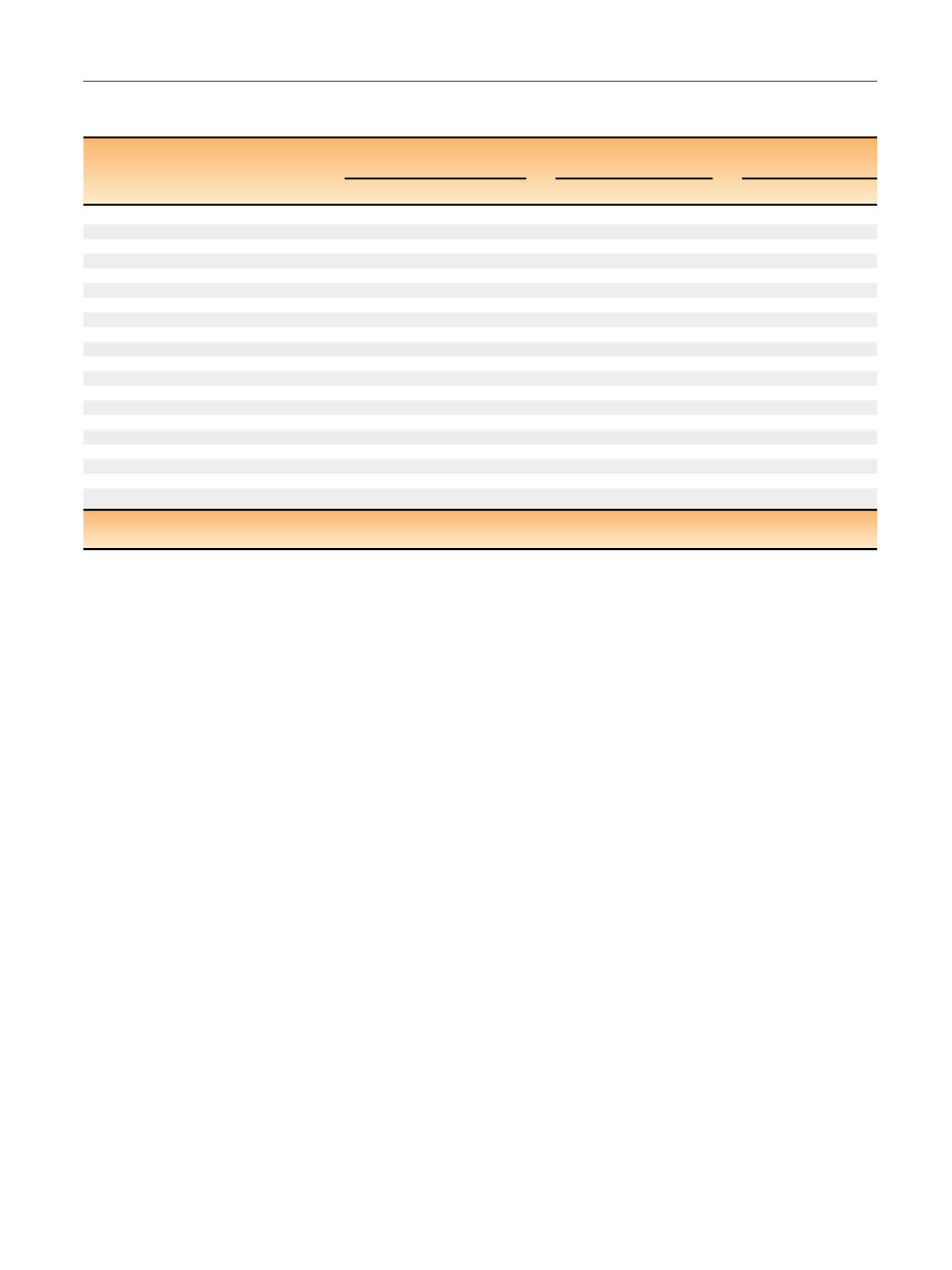
Table 5 – Clinical consequences showing the number of biopsies that could be avoided for initial surveillance biopsy or subsequent
surveillance biopsy
HGC probability
Biopsies
High-grade cancers
Primary Gleason
4 cancers
Performed
Avoided
Found
Missed
Found
Missed
Initial surveillance biopsy
Biopsy all
1000
0
214
0
44
0
Initial biopsy: risk by clinical variables + PSA
>
5%
943 (896–970)
57 (30–104)
214 (157–284)
0 (0–24)
44 (21–88)
0 (0–24)
>
10%
761 (689–821)
239 (179–311)
201 (146–270)
13 (3–45)
44 (21–88)
0 (0–24)
>
15%
509 (432–586)
491 (414–568)
164 (114–229)
50 (26–96)
38 (17–80)
6 (1–35)
Initial biopsy: risk by clinical variables + 4K
>
5%
956 (912–979)
44 (21–88)
214 (157–284)
0 (0–24)
44 (21–88)
0 (0–24)
>
10%
748 (676–809)
252 (191–324)
195 (141–263)
19 (6–54)
44 (21–88)
0 (0–24)
>
15%
522 (445–598)
478 (402–555)
182 (130–250)
31 (14–71)
44 (21–88)
0 (0–24)
Subsequent surveillance biopsies
Biopsy all
1000
0
147
0
47
0
Risk by clinical variables + PSA
>
5%
844 (789–886)
156 (114–211)
147 (105–201)
0 (0–18)
47 (26–85)
0 (0–18)
>
10%
692 (627–750)
308 (250–373)
133 (93–185)
14 (5–41)
43 (23–79)
5 (1–26)
>
15%
445 (380–513)
555 (487–620)
109 (74–158)
38 (19–73)
43 (23–79)
5 (1–26)
Risk by clinical variables + 4K
>
5%
848 (794–890)
152 (110–206)
142 (101–196)
5 (1–26)
47 (26–85)
0 (0–18)
>
10%
654 (588–715)
346 (285–412)
133 (93–185)
14 (5–41)
47 (26–85)
0 (0–18)
>
15%
408 (344–475)
592 (525–656)
100 (66–147)
47 (26–85)
38 (19–73)
9 (3–34)
HGC = high-grade cancer.
Results are presented as the number (95% confidence interval) per 1000 men.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 4 4 8 – 4 5 4
453
















