
At the time of first progression, 41% and 44% of patients
TBP and NTBP, respectively, had new lesions; lung was the
most common site in patients TBP and bone was the most
common site in patients NTBP. Patients TBP had fewer new
lesions in bone at first progression than those NTBP. Of
patients TBP and NTBP, 55% and 44%, respectively, had an
increase in target lesions
( Table 2). More patients TBP had
KPS 90 at first progression versus NTBP (73% vs 50%;
Table 2). With nivolumab, 17% and 27% of patients TBP and
NTBP, respectively, experienced deterioration in KPS at first
progression, and median QoL, measured by Functional
Assessment of Cancer Therapy-Kidney Symptom Index-
Disease Related Symptoms, was 32.0 and 27.0
( Table 2).
3.2.
Antitumor activity and OS after first progression
After first progression, median duration of nivolumab
treatment was 3.4 mo. Of patients TBP, 48% (74/153, 95%
CI: 40.2–56.6) had any tumor burden reduction and 13%
(20/153, 95% CI: 8.2–19.5) had 30% tumor burden
reduction after first progression
( Fig. 1A; note that 11 of
153 patients did not have tumor measurements before and
after first progression). A landmark analysis of OS beginning
from 4 wk postprogression to death in patients TBP and
NTBP with nivolumab demonstrated median OS (95% CI) of
20.4 (17.3–not reached) and 12.2 mo (9.5–14.6), respec-
tively (Supplementary Fig. 4). Median OS (95% CI) from
randomization in patients TBP and NTBP with nivolumab
was 28.1 (23.2–not reached) and 15.3 mo (13.0–18.3),
respectively.
Of the 153 patients TBP with nivolumab, 31 had a
complete or partial response, 51 had stable disease, and
70 had progressive disease as best overall response from
randomization to first progression (one patient did not
have
[2_TD$DIFF]
1 on-study assessment); 29 (complete or partial
response), 47 (stable disease), and 66 (progressive
disease) of these patients were evaluable and had tumor
measurements preprogression and postprogression. Of
the patients who had tumor measurements before and
after first progression and complete or partial response as
their best response before first progression, 28% (8/29)
had 30% tumor burden reduction during the treatment
beyond progression phase with nivolumab. In patients
with stable or progressive disease as their best response
before first progression, 6% (3/47) and 14% (9/66),
respectively, had 30% tumor burden reduction after
being TBP
( Fig. 1B–D). Tumor burden change over time
from randomization through treatment beyond progres-
sion is shown in
Fig. 2 .In an exploratory analysis of characteristics of patients
who responded (
[2_TD$DIFF]
30% tumor burden reduction,
n
= 20)
versus those who did not respond to treatment beyond first
progression (
n
= 133), a larger proportion who responded to
treatment beyond progression had a favorable Memorial
Sloan Kettering Cancer Center risk score (55% vs 35%),
presence of lung metastases (75% vs 44%), and the median
QoL was higher (33 vs 31;
Table 3).
Throughout the study, 83% (TBP) and 73% (NTBP) of
patients had a treatment-related adverse event (AE) with
nivolumab. By the first progression, treatment-related AEs
had occurred in 71% of patients TBP (8%, Grade 3 or 4) and
71% of patients NTBP (17%, Grade 3 or 4;
Table 4 ); the most
common was fatigue (31% [TBP] and 25% [NTBP];
Table 4 ).
After first progression, treatment-related AEs occurred in
59% of patients TBP (14%, Grade 3 or 4;
Table 4); the most
common was fatigue (20%).
4.
Discussion
This analysis from a large, international, phase 3 study is
consistent with results from the phase 2 study, demon-
strating that patients TBP with nivolumab resulted in
additional clinical benefit as evidenced by 13% of patients
experiencing a subsequent 30% decrease in tumor burden
[16]. Tumor burden reduction was observed in patients who
initially responded and then progressed, as well as in
patients with stable disease or progressive disease as their
best overall response (possibly due to tumor flare). Based on
RECIST criteria, some patients with progressive disease who
were subsequently TBP may have had a dissociated
response prior to first progression, with reduction or no
change in target lesions but presence of new lesions.
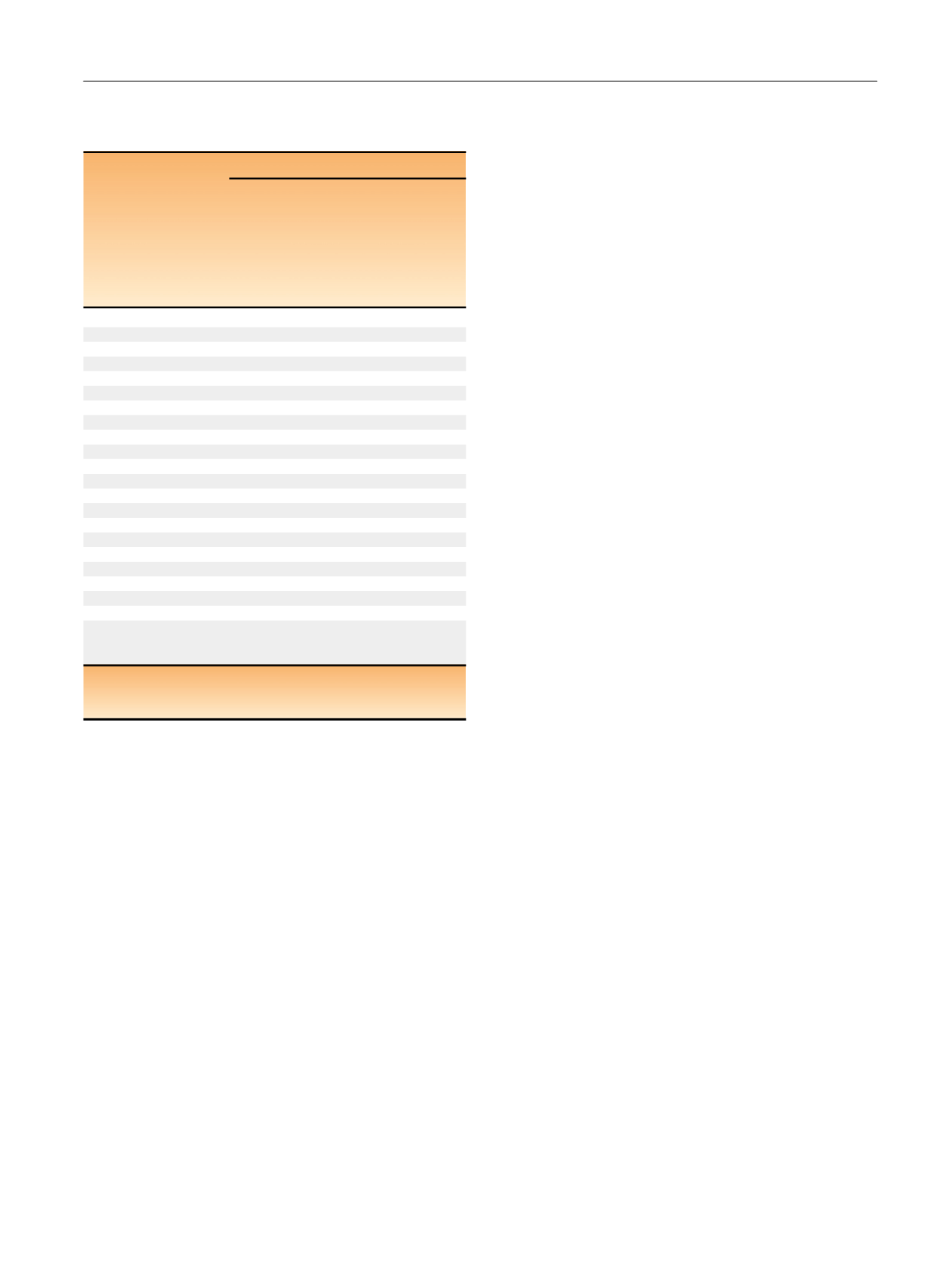
Table 3 – Baseline demographic and disease characteristics of
patients who responded versus those who did not respond to
treatment beyond progression
Nivolumab
Characteristics
Patients with
30% tumor
burden reduction
during treatment
beyond progression
(
n
= 20)
Patients with
<
30% reduction,
no reduction,
or increase in tumor
burden during
treatment beyond
progression
(
n
= 133)
Median age, yr (range)
60 (29–71)
62 (36–85)
KPS,
n
(%)
90
16 (80)
94 (71)
70 or 80
4 (20)
39 (29)
MSKCC risk group,
n
(%)
Favorable
11 (55)
47 (35)
Intermediate
8 (40)
62 (47)
Poor
0 (0)
24 (18)
Most common site of pretreatment target lesions,
n
(%)
Lung
15 (75)
58 (44)
Lymph node
7 (35)
46 (35)
Liver
3 (15)
30 (23)
No. of prior systemic antiangiogenic regimens,
n
(%)
1
16 (80)
97 (73)
2
4 (20)
36 (27)
Prior systemic regimen in metastatic setting,
n
(%)
Sunitinib
11 (55)
90 (68)
Pazopanib
3 (15)
33 (25)
Axitinib
2 (10)
14 (11)
Interleukin-2
2 (10)
9 (7)
Sorafenib
1 (5)
12 (9)
Quality of life (FKSI-DRS),
median (first quartile,
third quartile)
33.0 (31.0, 34.0)
31.0 (28.0, 34.0)
FKSI-DRS = Functional Assessment of Cancer Therapy-Kidney Symptom
Index-Disease Related Symptoms; KPS = Karnofsky performance status;
MSKCC = Memorial Sloan Kettering Cancer Center.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 3 6 8 – 3 7 6
371
















