
It was confirmed that saturation had been achieved by
the first 12 (out of 19) interviews in patients with DU
(without coexisting urological conditions). Further explo-
ration was required in the diagnostic groups that included
coexisting urological conditions
[7_TD$DIFF]
, as isolated minor concepts
were still being elicited. Ultimately, these were all
considered to be subconcepts of already elicited symptoms
or unlikely to be related to DU.
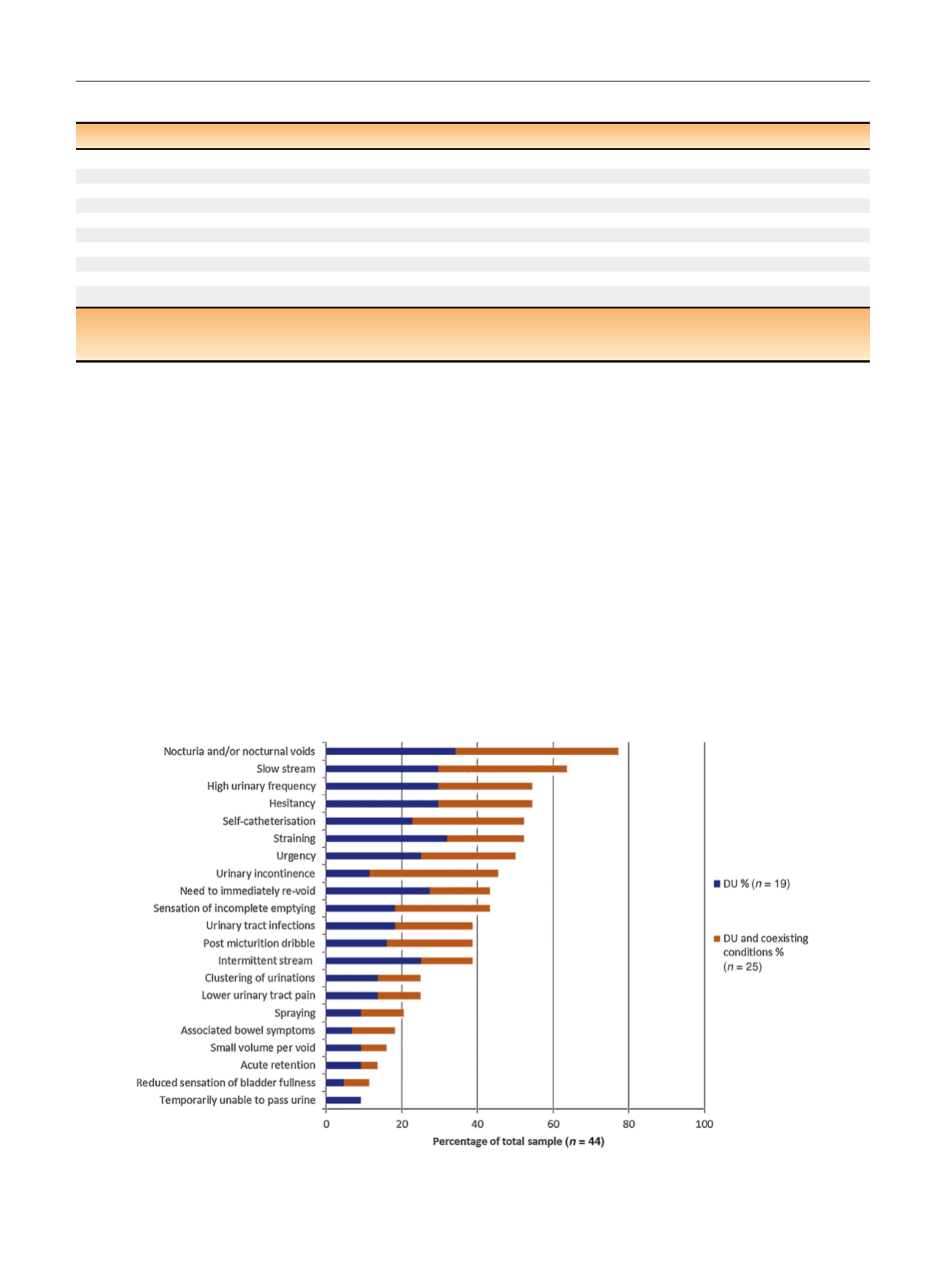
The
[1_TD$DIFF]
analysis revealed that patients reported a range of
LUTS that could have an associated impact on quality of life.
More than 20 storage, voiding, and other urological signs
and symptoms were described by the patients, as illustrated
in
Fig. 1, along with the indication of relative prevalence.
The following summarises the main findings and the
supplementary material online provides further detail
including additional representative quotes from the
patient’s accounts.
3.1.
Storage symptoms
The storage symptoms reported by over half of the patients
included nocturia, increased daytime frequency, and
urgency. These were reported by both sexes, often
spontaneously (without prompting) and frequently associ-
ated with a high degree of bother. Nocturia and/or nocturnal
voids was the most commonly reported overall symptom
(
n
= 34, 77%), as most patients described having to get out of
bed at least once in the night to urinate. Patients reported a
frequency of micturition from once or twice to over
12 urinations
[8_TD$DIFF]
every day. This was often associated with
urgency, the need to immediately revoid or
clustering
of
voids at certain times of the day. Urinary incontinence
occurred in all diagnostic groups and was very bothersome,
but was mainly associated with patients who demonstrated
DU and coexisting conditions (DO and stress urinary
Table 2 – Sample demographic and clinical characteristics
Clinical or demographic characteristic
Total sample
DU
DU + coexisting urological conditions
n
44
19
25
Mean age and range (yr)
64 (27–88)
59 (27–88)
68 (38–87)
Sex, male
n
(%)
29 (66)
12 (63)
17 (68)
Intermittent self-catheterisation,
n
(%) (historical or current)
23 (52)
10 (53)
13 (52)
PVR
>
30 m
l a , n(%)
34 (77)
14 (74)
20 (80)
PVR
>
30 m
l a , (ml; median and interquartile range)
199 (100–492)
335 (119–492)
170 (100–360)
BCI (median and interquartile range)
62 (49–79)
62 (48–82)
62 (50–77)
BOOI (median and interquartile range
) b18 (8–28)
15 (6–18)
25 (9–41)
p
det
Q
max
(cmH20; median and interquartile range)
25 (12–35)
24 (12–29)
26 (12–36)
Q
max
(ml/s; median and interquartile range)
8 (6–10)
8 (6–11)
6 (5–9)
BCl = bladder contractility index; BOOI = Bladder Outlet Obstruction Index; DU = detrusor underactivity; PVR = postvoid residual.
a
In the absence of any evidence base for the lower limit of a ‘‘significant’’ PVR we chose
>
30 ml.
b
Males only.
[(Fig._1)TD$FIG]
Fig. 1 – Prevalence of symptoms and signs reported in the total sample. The proportion reported by patients with detrusor underactivity (DU), and by
those with DU and coexisting urological conditions are shown.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 4 0 2 – 4 0 7
404
















