
70%, 4 + 3 in 10%, 8 in 1.8%, and 9 in 1.1%. GS upgrade was
therefore present in 156 patients (13%) and GS downgrade
in 201 (17%). A total of 295 men (25%) had unfavorable
disease at RP; 205 (17%) had non–organ-confined disease.
Using multivariable analysis, we looked at outcome
predictive features.
Table 3shows the results of this
analysis. For GS upgrade at definitive pathology, age (odds
ratio [OR]: 1.06; 95% confidence interval [CI], 1.03–1.09;
p
= 0.0007), PSAD (OR: 1.83; 95% CI, 1.17–2.85;
p
= 0.007),
and percentage of surface involvement (OR: 1.01; 95% CI,
1.00–1.02;
p
= 0.03) were the only elements reaching
statistical significance in the multivariable analysis. Peri-
neural invasion showed an OR of 1.37 (95% CI, 0.91–2.07)
without statistical significance (
p
= 0.13). PSAD (OR: 0.67),
higher cT (OR: 0.52), percentage of positive cores (OR: 0.98),
percentage of surface area (OR: 0.98), and perineural
invasion (OR: 0.59) were inversely associated with GS
downgrade. Age (OR: 1.05), clinical stage (OR: 1.74 for T2a),
percentage of positive cores
>
50% (OR: 1.57), percentage of
surface area (OR: 1.02), and perineural invasion (OR: 1.89)
were significant predictors of unfavorable disease at RP.
Increasing age, clinical stage, percentage of positive cores
50% (OR: 1.87), percentage of surface area, and the
presence of perineural invasionwere significantly associated
with the risk of non–organ-confined disease. HGPIN did not
show significant associations with pathologic outcomes
(data not shown).
4.
Discussion
Our data suggest that very favorable GS 3 + 4 IR men have a
relatively small but unpredictable risk of harboring higher
grade disease, and one in four patients may have unfavorable
disease features. GS downgrading is also fairly common in
this setting, and few clinical features can predict this
outcome.
The use of definitive RP pathology as a gold standard is a
distinctive feature of the present study, whereas many
previous works on risk reclassification were based on
repeated biopsy alone. All the pathologic material under-
went single-center review, and GS was assigned following
ISUP 2005 criteria in all cases. Given the high variability in
GS and upgrading criteria between different centers,
especially during the first years after the introduction of
the ISUP 2005 criteria
[9] ,we believe this is a significant
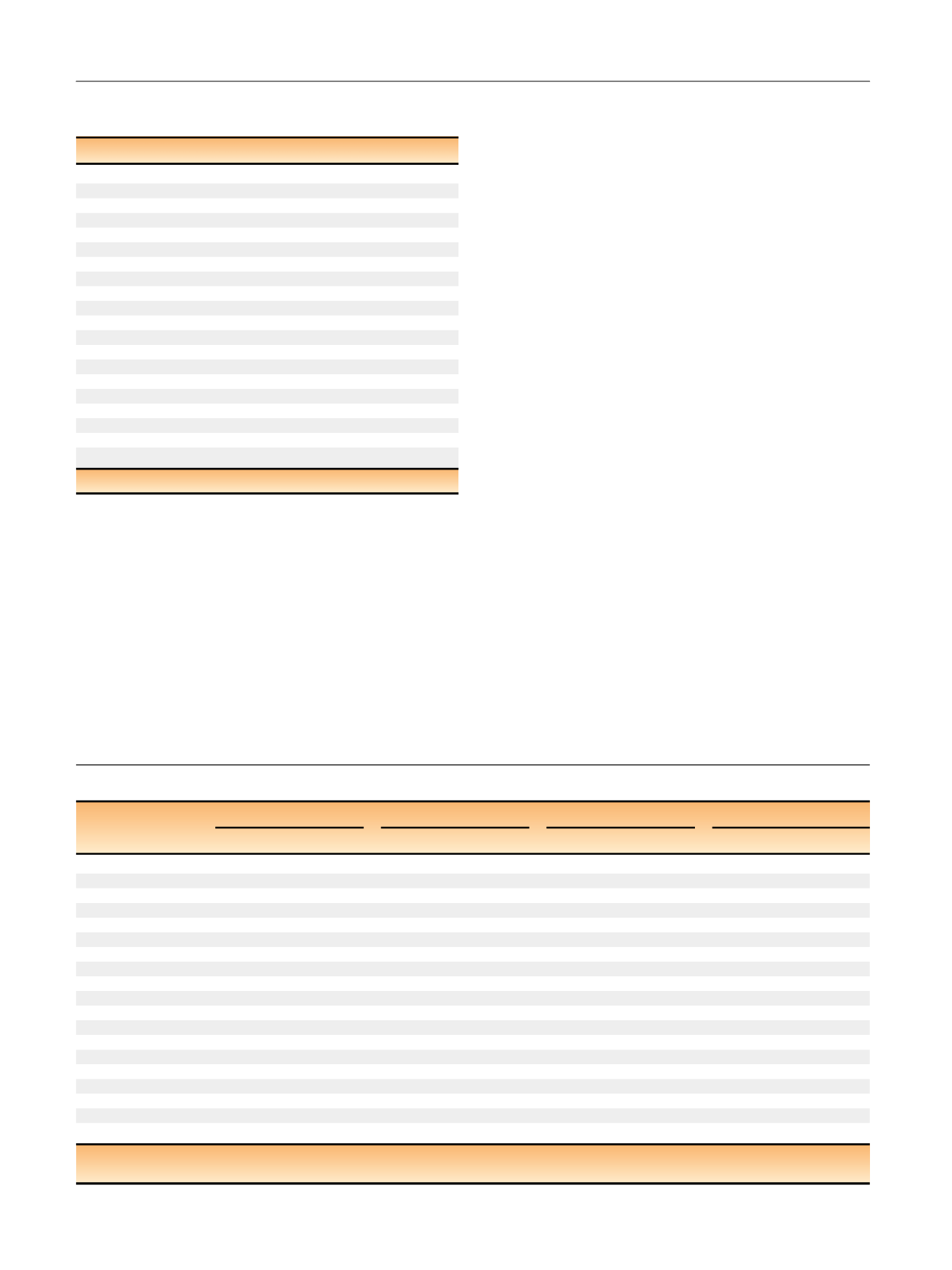
Table 3 – Multivariable analysis of outcome predictive features
Gleason upgrade
Gleason downgrade
Non–organ confined
Unfavorable disease
OR 95% CI
p
OR 95% CI
p
OR 95% CI
p
OR 95% CI
p
Age
1.06 1.02 1.09
<0.001
0.97 0.94 1.00 0.05 1.03 1.00 1.06
0.04
1.05 1.02 1.08
<0.001
Log
2
PSA density
1.83 1.17 2.85
0.007
0.67 0.51 0.89
0.006
1.04 0.79 1.35 0.79 1.14 0.90 1.44 0.29
Clinical stage
cT1
Ref.
Ref.
Ref.
cT2a
1.13 0.84 1.52 0.43 0.52 0.32 0.84
0.007
1.95 1.32 2.88
<0.001
1.74 1.23 2.46
0.002
Positive cores, % (cont) 0.99 0.99 1.01 0.55 0.98 0.97 0.99
0.007
1.02 1.01 1.03
<0.001
1.02 1.01 1.02
<0.001
Positive cores, %
<
50
ref
Ref.
Ref.
Ref.
50
0.96 0.57 1.62 0.88 0.76 0.45 1.28 0.3 1.87 1.22 2.85
0.004
1.57 1.06 2.31
0.02
Surface area, % (cont)
1.01 1.00 1.02
0.03
0.98 0.97 0.99
<0.001
1.02 1.01 1.03
<0.001
1.02 1.01 1.02
<0.001
Surface area, %
<
50
Ref.
Ref.
Ref.
Ref.
50
0.87 0.29 2.63 0.8 2.62 0.69 9.94 0.16 1.60 0.58 4.44 0.36 1.09 0.47 2.55 0.84
Tumor bilaterality
No
Ref.
Ref.
Ref.
Ref.
Yes
0.70 0.43 1.13 0.15 0.86 0.55 1.36 0.52 1.32 0.87 1.99 0.19 1.00 0.69 1.45 0.99
Perineural invasion
No
Ref.
Ref.
Ref.
Ref.
Yes
1.37 0.91 2.07 0.13 0.59 0.36 0.96
0.03
2.50 1.75 3.56
<0.001
1.89 1.36 2.62
<0.001
CI = confidence interval; OR = odds ratio; PSA = prostate-specific antigen; Ref = reference.
Boldface shows
p
<
0.05.
Table 2 – Pathologic and postoperative outcomes of the Gleason
score 3 + 4 very favorable intermediate-risk cohort
(
n
= 1190)
Pathologic T stage (%)
2a–b
274 (23)
2c
723 (61)
3a
144 (12)
3b
48 (4)
4
1 (0.1)
Pathologic GS (%)
6
201 (17)
3 + 4
833 (70)
4 + 3
121 (10)
8
22 (1.8)
9
13 (1.1)
GS upgrade (%)
156 (13)
GS downgrade (%)
201 (17)
Unfavorable disease (%)
295 (25)
Non–organ-confined disease (%)
205 (17)
Non–specimen-confined disease (%)
271 (23)
Positive surgical margin (%)
216 (18)
Positive lymph nodes (%)
20 (1.7)
Seminal vesicle invasion (%)
49 (4.1)
GS = Gleason score.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 4 4 2 – 4 4 7
444
















