
1.
Introduction
Whether or not active surveillance (AS) should be extended
to men with intermediate-risk (IR) prostate cancer (PCa) is a
highly debated issue. AS has emerged as a viable option for a
considerable number of men to counterbalance the risk of
overdiagnosis and overtreatment of clinically indolent
disease. Some AS protocols have included a small propor-
tion of men with Gleason score (GS) 7 disease
[1,2]and,
more recently, National Comprehensive Cancer Network
(NCCN) guidelines
[3]have listed AS an option for men with
‘‘favorable intermediate-risk’’ (FIR) PCa (GS 3 + 4, percent-
age of positive cores
<
50%, and only one additional IR
factor). However, most evidence supporting this risk
reclassification is indirect
[4], and many studies relied on
repeated biopsy results rather than on whole-specimen
pathology
[5] ,providing a partial perspective of the
complete picture. Since its introduction, GS has been
regarded as the single most important element in risk
assessment
[6] .Concerns about undergrading/staging at diagnosis and
missing the opportunity for cure if radical intervention is
delayed are the main drawbacks to the use of AS in the
setting of FIR PCa. Understanding the risk of harboring
unfavorable disease among this subgroup may foster more
appropriate selection of patients for AS protocols. The aimof
this study is to assess the risk of adverse characteristics in
men with very favorable risk GS 3 + 4 PCa and to identify
potential predictors of unfavorable features.
2.
Patients and methods
2.1.
Patient selection and evaluation
All patients with biopsy GS 3 + 4, prostate-specific antigen (PSA)
<
10 ng/ml, and clinical stage cT2a or lower who underwent radical
prostatectomy (RP) at our institution between 2006 and 2014 were
included in this retrospective cohort analysis. All had a histologically
confirmed diagnosis of PCa (transrectal prostate biopsy) within 3 mo
before surgery. Due to the referral nature of our practice, a pathologist at
our institution reviewed all the biopsy slides. Thus the biopsy GS score
reported represents the result of our internal review
[7], and detailed
biopsy information was available for all of the patients. RP was performed
using an open retropubic, laparoscopic, or robot-assisted approach by
experienced urologists. Pelvic lymph node dissection was carried out
according to the operating surgeons’ preferences. Surgical specimens were
processed and analyzed using a standardized technique, as previously
described
[8]. The institutional review board approved the study.
2.2.
Data collected
The clinical and biopsy variables included age at surgery, presurgery PSA,
PSA density (PSAD), clinical stage, primary and secondary Gleason grading
on biopsy, number of positive cores, number of total cores and percentage
of positive/total cores, maximum percentage of surface specimen tumor
involvement, presence of perineural invasion, and/or high-grade prostatic
intraepithelial neoplasia (HGPIN) in biopsy specimens.
Pathologic variables were primary and secondary GS, pT and pN
stage, and surgical margin status. American Joint Committee on Cancer
TNM 6th edition (2002) was used for pathologic staging, and GS was
assigned according to the 2005 International Society of Urological
Pathology (ISUP) modified Gleason scoring system
[9] .Upgrade was
defined as GS 4 + 3 at definitive pathology. Patients with advanced
pathologic stage (pT3–T4 and/or pN1) and/or a pGS 4 + 3 were
considered as ‘‘unfavorable disease’’ at RP
[10]. Pathologic stage pT2 or
lower and N0 was classified as ‘‘organ-confined disease,’’ whereas
‘‘specimen-confined disease’’ was pT2–pT3a PCa with negative margins
(R0) and negative lymph nodes (pN0)
[11] .2.3.
Statistical analysis
In addition to descriptive statistics, we used the chi-square test for
comparing categorical variables and the Student
t
test or Wilcoxon rank
sum test for comparison of continuous variables. Clinical data (age,
PSAD, with logarithmic transformation, and clinical stage) and detailed
biopsy information were analyzed in multivariable prediction models
using logistic regression. The percentage of positive cores/total and
percentage of specimen surface tumor involvement were considered
both as continuous values and categorized as
<
50% or 50%, in
accordance with the cut-off suggested by the recent NCCN guidelines
update
[3]. All tests were two sided with
a
value of 0.05.
3.
Results
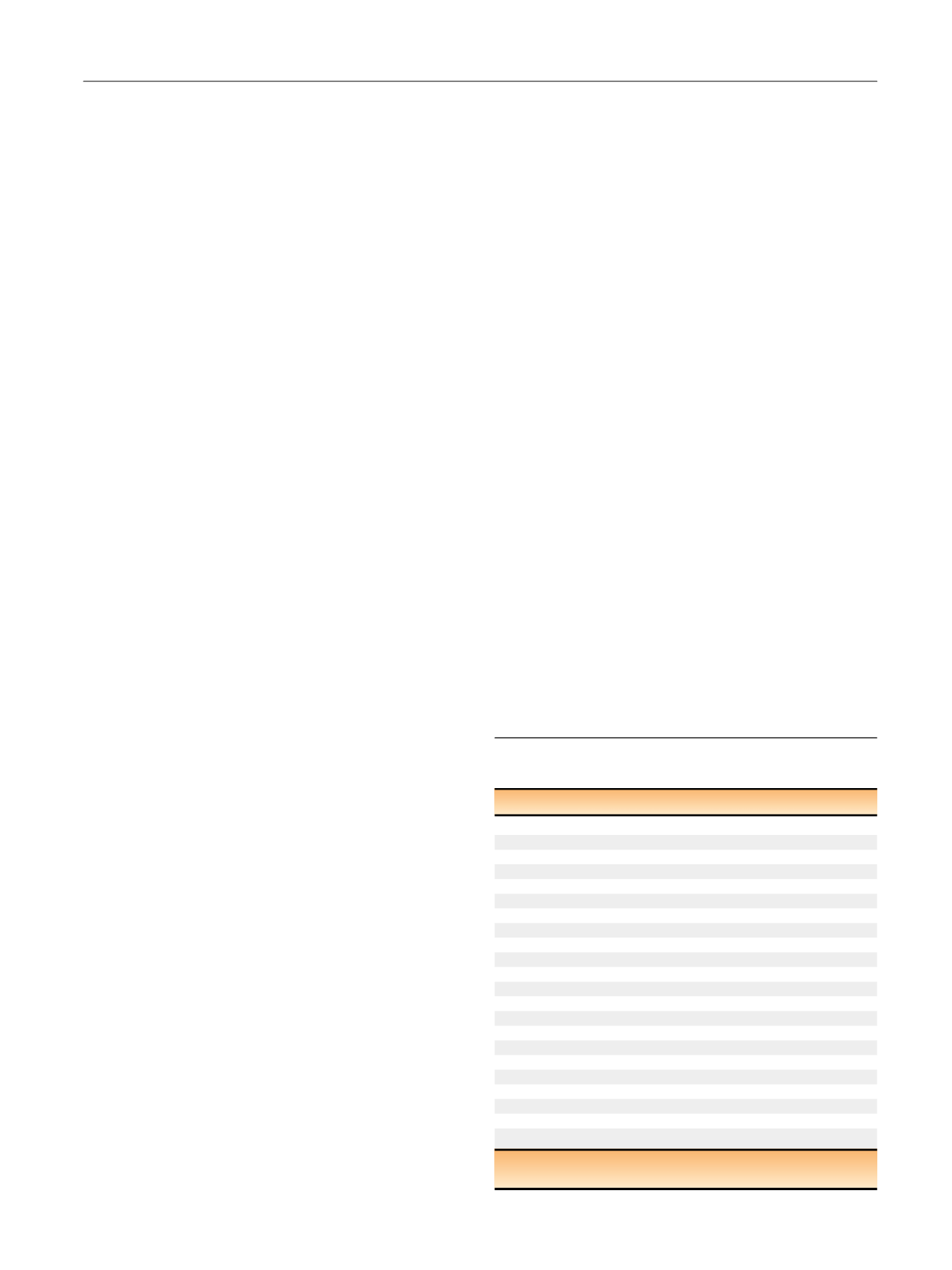
A total of 1190 patients were included.
Table 1shows the
baseline demographic and clinical features of the cohort.
Median age at surgery was 62 yr (interquartile range
[IQR]: 57–67); PSA was 5.2 ng/ml (IQR: 4.3–6.6). The cT
stage was T1 in 812 patients (68%) and T2a in 378 (32%).
Median percentage of positive cores was 33% (IQR: 19–50),
and median surface area percentage of involvement was
25% (IQR: 10–50); perineural invasion was present in
273 patients (23%).
Table 2lists the pathologic outcomes of the cohort. The
pT stage was 2a–2b in 274 (23%), 2c in 723 (61%), 3a in 144
(12%), and 3b in 48 (4%). Pathologic GS was 6 in 17%, 3 + 4 in
Table 1 – Demographic and preoperative features of the Gleason
score 3 + 4 very favorable intermediate-risk cohort
(
n
= 1190)
Age at surgery, yr
Median (IQR)
62 (57–67)
Range
37–79
Preoperative PSA, ng/ml
Median (IQR)
5.2 (4.3–6.6)
Clinical T stage (%)
T1c
812 (68)
T2a
378 (32)
Total biopsy cores
Median (IQR)
12 (12–14)
Positive biopsy cores
Median (IQR)
4 (3–6)
Positive cores, %
Median (IQR)
33 (19–50)
Surface area, %
Median (IQR)
25 (10–50)
HGPIN (%)
No
1064 (89)
Yes
126 (11)
Perineural invasion (%)
No
916 (77)
Yes
274 (23)
HGPIN = high-grade prostatic intraepithelial neoplasia; IQR = interquartile
range; PSA = prostate-specific antigen.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 4 4 2 – 4 4 7
443
















